
How many people have HIV in the United States?
The CDC estimates at the end of 2017, there were 1,018,346 adults and adolescents with diagnosed HIV in the US and dependent areas. Since 2010, the number of people living with HIV has increased, while the annual number of new HIV infections has declined to 37,832 diagnosed in 2018.
How many HIV medications are available today?
Today, more than 30 HIV medications are available. Many people are able to control their HIV with just one pill a day. Early treatment with antiretrovirals can prevent HIV-positive people from getting AIDS and the diseases it causes, like cancer. HIV drugs also stop people who have the virus from passing it to their partner during sex.
What percentage of people with HIV are treated within 1 month?
76% of people who received an HIV diagnosis in 2016 were linked to HIV medical care within 1 month. In 2015, among all adults and adolescents with diagnosed HIV, 73% received some HIV medical care, 57% were retained in continuous HIV care, and. 60% had achieved viral suppression.
How many people die of HIV/AIDS each year?
As of 2016, about 675,000 people have died of HIV/AIDS in the U.S. since the beginning of the HIV epidemic. With improved treatments and better prophylaxis against opportunistic infections, death rates have significantly declined.
How many people are being treated for HIV?
HIV Treatment Access—As of June 2020, 28.2 million people with HIV (75%) were accessing antiretroviral therapy (ART) globally. That means 9.5 million people are still waiting. HIV treatment access is key to the global effort to end AIDS as a public health threat.
What percent of the United States population has HIV?
WASHINGTON (Reuters) - About one-half of one percent of young adults living in homes in the United States are infected with the AIDS virus, around 600,000 people, the National Center for Health Statistics reported on Tuesday.
How many people have HIV in the US today?
Today, there are more than 1.2 million people living with HIV in the U.S. and there are more than 35,000 new infections each year. people with AIDS have died since the beginning of the epidemic. More than 700,000 people in the U.S., have died from HIV-related illness.
Who has the highest rate of HIV in the US?
Black/African Americanj and Hispanic/Latinok people are disproportionately affected by HIV. In 2019: Black/African American people accounted for 42% (15,305) of new HIV diagnoses and 13% of the population. Hispanic/Latino people accounted for 29% (10,494) of new HIV diagnoses and 18% of the population.
How many people have HIV in 2019?
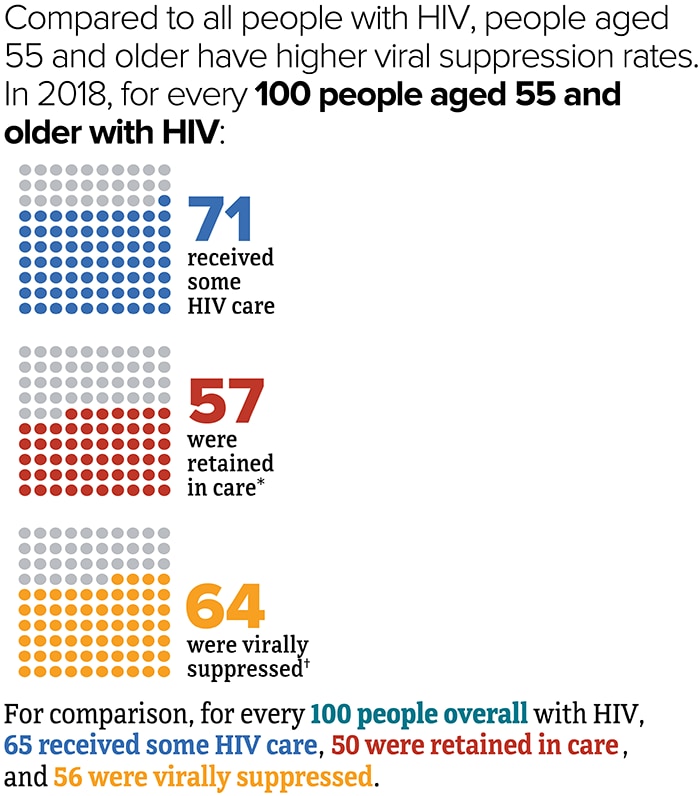
According to another CDC report, of the estimated 1.2 million people with HIV (diagnosed and undiagnosed) in 2019, about 65.9% received some HIV care, 50.1% were retained in care, and 56.8% were virally suppressed or undetectable.
How many new HIV cases were there in 2019?
In 2019, an estimated 34,800 new HIV infections occurred in the United States.
What is the incidence of HIV?
HIV incidence refers to the estimated number of new HIV infections during specified period of time (such as a year), which is different from the number of people diagnosed with HIV during a given year.
What is the highest rate of HIV in 2019?
In 2019, the highest rate was for Blacks/African American persons (42.1), followed by Hispanic/Latino persons (21.7) and persons of multiple races (18.4). By sex at birth, the annual number of new HIV infections in 2019, as compared to 2015, decreased among males, but remained stable among females.
Where are HIV diagnoses concentrated?
Most diagnoses are now highly concentrated in certain geographic areas. More than 50 percent of new HIV diagnoses in 2016 and 2017 occurred in 48 counties, Washington, D.C., and San Juan, Puerto Rico. These 50 jurisdictions are prioritized in Phase I of Ending the HIV Epidemic: A Plan for America, along with seven states with a disproportionate occurrence of HIV in rural areas.
What age group is the highest in HIV?
By age group, in 2019, the number of new HIV diagnoses was highest among people aged 25 to 29.
How long can you live with HIV?
(Some people can live with HIV for years before they are diagnosed; others are diagnosed soon after acquiring HIV.)
How many people have been infected with HIV?
Since the first cases of HIV were reported back in 1981, an estimated 76 million people have been infected worldwide, resulting in over 22 million deaths and 13 million AIDS orphans. 1 .
How many new HIV cases were reported in 2019?
According to data from the Centers for Disease Control and Prevention (CDC), 37,968 new HIV infections were reported in the 2019 surveillance—a drop of nearly 8% since 2010. 3
What are the driving factors for HIV failure?
HIV stigma and a lack of access to medical care, particularly among the poor and communities of color, are among the driving factors for these failures. 4
How much is the black MSM at risk of HIV?
Due to the multitude of intersecting risk factors, Black MSM in the United States have no less than a 50% lifetime risk of getting HIV, according to a 2018 study in the Annals of Epidemiology. 15 .
Why are black women more likely to get HIV than white women?
The risk is especially high among Black women due to socioeconomic and gender inequalities. As a result, a Black woman is 13 times more likely to get HIV than a White woman of the same age. (By contrast, White women are more than twice as likely to get infected as a result of injecting drug use compared to Black women). 16
What is the cause of death for HIV?
HIV causes the depletion of immune cells (called CD4 T-cells) that, over time, reduces a person's ability to fight otherwise harmless infections. When the immune defenses have been fully compromised , these infections can become life-threatening. It is these so-called opportunistic infections that are among the main causes of death in people living with HIV.
How much has HIV dropped since 2004?
Since the height of the pandemic in 2004, HIV-related deaths and have dropped by no less than 60%, while the rate of mother-to-child transmission has been cut in half. 3 . BigFive Images / Gallo Images / Getty Images.
How many people died from HIV in 2018?
In 2018, there were 15,820 deaths among adults and adolescents with diagnosed HIV in the US and dependent areas. These deaths may be due to any cause. a HIV diagnoses refers to the number of people who received an HIV diagnosis during a given time period, not when the people got HIV infection.
Which group is most affected by HIV?
Black/African American j and Hispanic/Latino k people are disproportionately affected by HIV. In 2019:
What is HIV diagnosis?
HIV diagnoses is one of the six Ending the HIV Epidemic in the U.S. indicators. HIV diagnoses refers to the number of people who received an HIV diagnosis during a given year.
When did HIV diagnoses stabilize?
From 2015 to 2019, HIV diagnoses were stable among people who inject drugs overall.
How many states are there in the US?
l The US Census Bureau’s population estimates include the 50 states, the District of Columbia, and Puerto Rico.
Can HIV be undetectable?
Taking HIV medicine every day can make the viral load undetectable. People who get and keep an undetectable viral load (or stay virally suppressed) can live a long and healthy life. They also have effectively no risk of transmitting HIV to HIV-negative sex partners. Download and Share This Infographic. image icon.
Is HIV evenly distributed in the US?
HIV diagnoses are not evenly distributed regionally in the US and dependent areas .
How many people in the world have HIV?
According to the World Health Organization, there are about 37.9 million people in the world living with HIV in 2018. The prevalence of HIV in adults ages 15 to 29 is estimated at about 0.8% of the world’s population.
Which state has the highest HIV rate?
California has the highest number of people living with HIV of 128,153, a rate of 389.7 people with HIV per 100,000 residents. Of those living with HIV in California, the largest group is White with 48,155 people and the second-largest is Hispanic/Latino with 48,029.
How does HIV spread?
HIV is spread through body fluids such as blood. If HIV goes untreated and advances, it can lead to acquired immunodeficiency syndrome or AIDS. Unlike most other viruses, when a person contracts HIV, they have it for life because the human body cannot fight off the virus entirely.
What are the stages of HIV?
Unlike most other viruses, when a person contracts HIV, they have it for life because the human body cannot fight off the virus entirely. HIV, however, can be controlled and its progression can be slowed significantly. There are three stages of HIV: 1 Acute HIV infection 2 Clinical latency (HIV inactivity or dormancy) 3 AIDS
What is the UNAIDS program?
UNAIDS, the Joint United Nations Program on HIV/AIDS, is the world’s leading advocate for the comprehensive and coordinated global action against the HIV/AIDS pandemic. In 2014, UNAIDS established the 90-90-90 goals, which called for countries around the world to get 90% of people living with HIV diagnosed; 90% of those diagnosed accessing treatment, and 90% of people on treatment to have suppressed viral loads by 2020.
How does ART help with HIV?
ART reduces the viral load (amount of the virus) in the body’s blood and fluids. ART can not only slow the progression of HIV but also reduces the chances of transmitting the virus to other people. ART is recommended for all people diagnosed with HIV and should be started as soon as possible after diagnosis.
What is the HIV rate in Florida?
Florida’s HIV rate is 612.3 per 100,000. The group with the highest number of people living with HIV is Black/African American with 49,943. Texas has the fourth-highest number of people living with HIV in the United States of 88,099, translating to a rate of 382.9 per 100,000 people.
How many different HIV treatments were there in 2010?
Researchers continued to create new formulations and combinations to improve treatment outcome. By 2010, there were up to 20 different treatment options and generic drugs, which helped lower costs. The FDA continues to approve HIV medical products, regulating: product approval. warnings.
Who was the only person to have been cured of HIV?
Brown, a Seattle native living in Berlin at the time of his treatment, was the only person who’d been successfully cured of HIV until a similar case was revealed in 2019. Adam Castillejo, originally identified as “the London patient,” had also received a stem cell transplant to help treat cancer.
What was the public response to the AIDS epidemic?
Public response was negative in the early years of the epidemic. In 1983, a doctor in New York was threatened with eviction, leading to the first AIDS discrimination lawsuit. Bathhouses across the country closed due to high-risk sexual activity. Some schools also barred children with HIV from attending.
What is the FDA approved drug for HIV?
Recent drug development for HIV prevention. In July 2012, the FDA approved pre-exposure prophylaxis (PrEP). PrEP is a medication shown to lower the risk of contracting HIV from sexual activity or needle use. The treatment requires taking the medication on a daily basis.
How many people died from AIDS in 1995?
By 1995, complications from AIDS was the leading cause of death for adults 25 to 44 years old. About 50,000 Americans died of AIDS-related causes.
What is PrEP in HIV?
PrEP is shown to reduce the risk for HIV infection by greater than 90 percent.
Where did HIV come from?
One sample was drawn as far back as 1959 from a man living in what’s now known as the Democratic Republic of the Congo.
Where do HIV patients get their services?
Some patients receive services directly at the health center itself, while others are referred to an HIV specialist in the community. Major investments in the network of community health centers over the past several years have created more opportunities for HIV care delivery.
What is Medicare for HIV?
Medicare —Medicare is health insurance for people age 65 or older, people under 65 with certain disabilities, and people of all ages with End-Stage Renal Disease. Medicare coverage for eligible individuals includes outpatient care, prescription drugs, and inpatient hospital care. It covers all medically necessary treatment for a person with HIV. To learn more about Medicare coverage and choices, visit Medicare.gov.
What is Ryan White HIV?
The Ryan White HIV/AIDS Program —The Ryan White HIV/AIDS Program works with cities, states, and local community-based organizations to provide HIV-related services to more than half a million people living with HIV each year. The program is for those who do not have sufficient health care coverage or financial resources to cope with HIV disease. Ryan White fills gaps in care not covered by these other sources. The program is divided into several “parts” to meet the needs of different communities and populations, and includes support for an AIDS Drug Assistance Program (ADAP). To find a Ryan White clinic near you, use the HIV.gov HIV Services Locator.
What is the Indian Health Service?
American Indian and Alaska Native Programs —The Indian Health Service (IHS) provides health care services—including HIV services —for members and descendants of federally-recognized American Indian and Alaska Native Tribes. For more information, go to https://www.ihs.gov.
Why is it important to treat viral infections?
These things are important because with the proper care and treatment, you can reduce your viral load, protect your health, enjoy a long and healthy life, and reduce the potential of transmitting the virus to others. But you might have concerns about how to pay for this. There are resources that can help you pay for the care you need.
What is the VA?
Veterans Programs —The Veterans Administration (VA) is the largest single provider of medical care to people living with HIV in the U.S., supporting over 24,000 Veterans living with HIV. If you are eligible, you may be able to receive HIV care through the Veterans Health Administration.
How prevalent is HIV in prisons?
A generalized epidemic of HIV persists among the incarcerated U.S. population. Overall, the HIV seroprevalence among incarcerated individuals is 1.5%, approximately 3 times greater than among the general U.S. population.(1) Although the prevalence of HIV in prisons has decreased since the late 1990s, concomitant increases in the size of the incarcerated population have led to a constant number of HIV cases in correctional facilities.(2) The HIV prevalence in the state prisons of Florida, Maryland and New York exceeds 3%, a rate higher than the national prevalence of any country outside of sub-Saharan Africa.(3)
What is HIV/AIDS disproportionately involved in?
People living with HIV/AIDS are disproportionately involved in the criminal justice system , and often have complex medical, mental health, and substance abuse needs.
Why is clinical research important in prison?
Clinical research involving inmates in jails or prisons is fraught with ethical challenges. Since inmates bear a disproportionate burden of HIV infection, it is important and justifiable that researchers investigate issues related to HIV care and prevention in as they relate to incarcerated persons. Yet the barriers to conducting ethical research in correctional settings are daunting. Because inmates are by nature in a coercive environment, the autonomy to provide voluntary consent may be limited. Coercion may be actual or may be perceived.(86) Incarceration by its nature, limits choices. Inmates may feel that may not receive needed care if they decline to participate in clinical studies. For these reasons, federal regulations provide safeguards that federally funded clinical research among inmates must follow. These are found in 45 CFR 46, Subpart C, and apply to all research involving any individual who is or becomes a prisoner while participating in a study. (Table 1) The intent of these regulations is laudable, but the practical effect has been to discourage clinical research that could be of great benefit. Even when clinical research is approved, numerous challenges remain. Confidentiality and privacy are in short supply in prisons and jails.(86) Both the physical environment and policies and procedures may limit privacy.(87) Attitudinal and structural barriers to research are frequently encountered. For example, correctional officers may not perceive the value of clinical research, and hence may put up “roadblocks”. Structural barriers such as the “count” of inmates each shift may limit the time for interviews. Clinical research within corrections requires enormous personal effort and time to fulfill ethical and regulatory requirements. Yet it is very worthwhile because of the huge benefit that may accrue from such research. Improved diagnosis, treatment, or even prevention of substance abuse, mental illness, and infectious diseases such as HIV that disproportionately impact incarcerated communities would be of great value.
Why is HIV incarcerated?
For people living with HIV who receive care in the community, incarceration, by virtue of its inherent disruption of social networks and patient-provider relationships , is a major impediment to effective, longitudinal HIV care. Among injection drug users, incarceration is a major reason for discontinuation of ART,(56) decreased adherence to ART,(52, 57) and is associated with decreased likelihood of viral suppression among ART initiators.(58, 59) Furthermore, among individuals successfully achieving viral suppression in the community, incarceration is strongly associated with plasma HIV RNA rebound.(60, 61)
Why is HIV testing low in prison?
In prisons, where slower turnover makes testing more feasible, low rates of HIV testing may result from lack of institutional policies or protocols that guide providers’ decisions to offer testing in a standardized way. In prisons as well as jails, an “opt-out” strategy to HIV testing has numerous advantages to traditional approaches that rely upon the discretion of providers or the initiative of patients. A review of prison-based testing in North Carolina demonstrated that 60% of individuals with HIV risk factors were never tested.(30) After that prison system implemented a routine, opt-out testing strategy, the proportion of inmates tested and the number of new diagnoses promptly and dramatically increased.(31) The Washington Department of Corrections found that inmate request led to 5% of incoming male prisoners tested.(32) An opt-in testing policy resulted in 72% of incoming inmates receiving testing; a further change to opt-out testing led to 90% of entrants tested. Because a prison system is responsible for providing healthcare to its entrants for a period of years, aggressive opt out testing for HIV is important, so that appropriate medical care can be delivered.
Does the CDC recommend HIV testing?
Since 2006 the U.S. Centers for Disease Control and Prevention (CDC) has recommended routine HIV testing for adults in all clinical settings, including correctional facilities.(15, 16) As described in previous reviews, numerous logistical challenges have resulted in missed opportunities to conduct testing among people who are incarcerated, but experience in some jurisdictions demonstrates how testing can be feasibly and efficiently expanded.(17, 18) A national survey of prison and jail systems suggested 39% of prisons do mandatory or routine HIV testing and only 36% of jails offer any HIV testing.(19) A study of individual jail detainees found that fewer than 1 in 4 had been tested for HIV at any time during their current detention.(20)
Should HIV testing be done in jail?
The evidence reviewed above makes a strong case for universal, opt-out testing in the jails of cities with high HIV prevalence. Universal testing may not be cost-effective or appropriate in all jurisdictions, however, and it is reasonable to consider tailoring jail screening practices based on prevalence in the catchment area or among cohorts entering the institution in the recent past. The appropriate threshold below which routine testing can be deferred has not been defined, although CDC suggests it ought to be very low, recommending that “correctional facilities should provide detainees with routine opt-out HIV testing, unless the prevalence of previously undiagnosed HIV infection has been documented to be less than 0.1%.”(39)
How many HIV medications are there?
Today, more than 30 HIV medications are available. Many people are able to control their HIV with just one pill a day. Early treatment with antiretrovirals can prevent HIV-positive people from getting AIDS and the diseases it causes, like cancer.
What is the name of the drug that is used to treat HIV/AIDS?
These drugs paved the way to a new era of combination therapy for HIV/AIDS. Doctors began prescribing saquinavir plus AZT or other antiretrovirals. This combination therapy was dubbed highly active antiretroviral therapy (HAART). That approach became the new standard of care for HIV in 1996. HAART greatly lengthened the life span of people with AIDS.
What drug stopped HIV from multiplying?
Also called azidothymidine (AZT), the medication became available in 1987.
What is the name of the drug that shuts down HIV?
Similar to AZT, NNRTIs shut down HIV by targeting the enzymes it needs to multiply. These drugs paved the way to a new era of combination therapy for HIV/AIDS.
When did the FDA approve the pill Combivir?
The multiple doses and the drugs’ side effects drove many people to quit their HIV therapy. Then in 1997 , the FDA approved a pill called Combivir that contained two anti-HIV drugs and was easier to take. Nearly 2 decades after the emergence of HIV and AIDS, a dozen antiretroviral drugs were on the market. PrEP.
When did the FDA approve Truvada?
In 2012, the FDA approved the drug Truvada for pre-exposure prophylaxis, or PrEP.
When was AIDS discovered?
In 1983 , scientists discovered the virus that causes AIDS. They later named it human immunodeficiency virus (HIV). The race was on for a treatment to stop this deadly disease.
How many new cases of HIV in 2017?
The most recent CDC HIV Surveillance Report estimates that 38,281 new cases of HIV were diagnosed in the United States in 2017, a rate of 11.8 per 100,000 population. This rate is a decrease from the previous year's estimates, which indicated 39,589 new infections and a rate of 12.2 per 100,000 population. Individuals in the age range 25–29 years-old had the highest rates of new infection, with a rate of 32.9 per 100,000. With regard to race and ethnicity, the highest rates of new infections in 2017 occurred in the black/African-American population, with a new infection rate of 41.1 per 100,000. This more than doubled the next highest rate for a racial or ethnic group, which was Hispanic/Latino with a rate of 16.6 per 100,000. The lowest rates of new infection in 2017 occurred in the white population and Asian population, which each had a new infection rate of 5.1 per 100,000.
Why did the AIDS activist groups take initiative in testing and experimenting with new possible medications for treating HIV?
Initially when the AIDS epidemic surface d in the United States, a large proportion of patients were LGBT community members, leading to stigmatization of the disease. Because of this, the AIDS activist groups took initiative in testing and experimenting with new possible medications for treating HIV, after researchers outside of the community refused. This research originally done by early activist groups contributed to treatments still being used today.
What was the AIDS movement?
Starting in the early 1980s, AIDS activist groups and organizations began to emerge and advocate for people infected with HIV in the United States. Though it was an important aspect of the movement, activism went beyond the pursuit of funding for AIDS research. Groups acted to educate and raise awareness of the disease and its effects on different populations, even those thought to be at low-risk of contracting HIV. This was done through publications and "alternative media" created by those living with or close to the disease.
What is the goal of the National HIV/AIDS Strategy?
In 2010, President Obama created the National HIV/AIDS Strategy for the United States (NHAS), with its three main objectives being to reduce the annual number of infections, reduce health disparities, and increase access to resources and HIV care.
How many HIV hotspots did Trump have in 2019?
The Department of Health and Human Services issued grants to 32 HIV "hotspots" in 2019, and Congress earmarked over $291 million for the president's plan in FY2020.
How many Hispanics died from AIDS in 2016?
Since the epidemic began, more than 100,888 Hispanics/Latinos with an AIDS diagnosis have died, including 2,863 in 2016. American Indian/Alaskan Native communities in the United States see a higher rate of HIV/AIDS in comparison to whites, Asians, and Native Hawaiians/other Native Pacific Islanders.
What were the responses to the 1980s AIDS epidemic?
These included new medical treatments, travel restrictions, and new public health policies in the United States.
Fast Facts
- Approximately 1.2 million people in the U.S. have HIV. About 13 percent of them don’t know it and need testing.
- HIV continues to have a disproportionate impact on certain populations, particularly racial and ethnic minorities and gay, bisexual, and other men who have sex with men.
- In 2019, an estimated 34,800 new HIV infections occurred in the United States.
- Approximately 1.2 million people in the U.S. have HIV. About 13 percent of them don’t know it and need testing.
- HIV continues to have a disproportionate impact on certain populations, particularly racial and ethnic minorities and gay, bisexual, and other men who have sex with men.
- In 2019, an estimated 34,800 new HIV infections occurred in the United States.
- New HIV infections declined 8% from 37,800 in 2015 to 34,800 in 2019, after a period of general stability.
New HIV Infections
- HIV incidence refers to the estimated number of new HIV infections during specified period of time (such as a year), which is different from the number of people diagnosedwith HIV during a given year. (Some people may have HIV for some time but not know it, so the year they are diagnosed may not be the same as the year they acquired HIV.) According to the latest estimate…
HIV Diagnoses
- HIV diagnoses refers to the number of people who have received an HIV diagnosis during a year, regardless of when they acquired HIV. (Some people can live with HIV for years before they are diagnosed; others are diagnosed soon after acquiring HIV.) According to the latest CDC data, in 2019, 36,801 people received an HIV diagnosis in the United Stat...
Living with HIV
- At year-end 2019, an estimated 1.2 million people in the United States aged 13 and older had HIV in the U.S., the most recent year for which this information is available. According to the latest CDC data: 1. About 13% of people with HIV in the U.S. don’t know it and so need testing. Early HIV diagnosis is crucial. Everyone aged 13-64 should be tested at least once. People at higher risk o…
Deaths
- In 2019, there were 15,815 deaths among adults and adolescents with diagnosed HIV in the United States and 6 dependent areas. These deaths may be due to any cause.
Need More?
- For information about how HIV affects your state or county, visit America’s HIV Epidemic Analysis Dashboard (AHEAD), an interactive dashboard that lets you examine data for six Ending the HIV Epidemic indicators that measure both local and national progress toward ending the U.S. HIV epidemic by 2030. With AHEAD, you can filter data several different ways and compare data acr…
Notes
- a Unless otherwise noted, the term United States (U.S.) includes the 50 states, the District of Columbia, and the 6 dependent areas of American Samoa, Guam, the Northern Mariana Islands, Puerto Rico, the Republic of Palau, and the U.S. Virgin Islands. b The term male-to-male sexual contact is used in CDC surveillance systems. It indicates a behavior that transmits HIV infection…
Bibliography
- CDC. Diagnoses of HIV Infection in the United States and Dependent Areas, 2019. HIV Surveillance Report 2021; 32. CDC. Estimated HIV incidence and prevalence in the United States, 2015-2019. HIV Surveillance Supplemental Report 2021; 26(No. 1) CDC. Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data—United States and …
HIV in The United States
HIV Infections by State
- In the United States, where you live plays a large part in how likely you are to get HIV. While it is clear that dense urban populations with high prevalence ratescontribute to the risk, there are other unique factors that account for a growing disparity between U.S. states. A prime example is the rate of infection in states that have either adopted or refused Medicaidexpansion, intended to ex…
by Age
- In the United States, the primary mode of HIV transmission is sex. It can come as no surprise, therefore, that the rates of new infection are highest among younger populations that are not only more sexually active but also more likely to have STDs, multiple sex partners, and other risk factors. According to the CDC, the rate of new infections is highest among people 13 to 29, decli…
by Sexual Orientation
- Gay and bisexual men account for the lion's share of HIV infections in the U.S. This not only includes men who identify as gay or bisexual but the nearly one in 10 men who have sex with men (MSM) who identify as straight.8 While MSM accounts for only 2% of the U.S. population, they represent 69% of all new infections and 55% of Americans living with HIV. In their 2018 surv…
by Race
- HIV and race are integrally linked, with people of color disproportionately affected. There are many reasons for this, not least of which are the economic disparities and lack of access to quality healthcare in many ethnic and racial communities.4 This is especially true among Blacks in the United States whose new infection rate outpaces that of Whites by 34%.7 Currently, there …
by Sex
- Although men account for the majority of HIV infections in the U.S.—75% of whom are MSM—there are around 258,000 women living with HIV, the majority of whom were infected through heterosexual sex.16 As the receptive partner in a heterosexual couple, women are twice as likely to get HIV as their male partners. This is reflected by data published by the CDC in 2018…
Mortality Rates
- HIV causes the depletion of immune cells (called CD4 T-cells) that, over time, reduces a person's ability to fight otherwise harmless infections. When the immune defenses have been fully compromised, these infections can become life-threatening. It is these so-called opportunistic infectionsthat are among the main causes of death in people living with HIV. In the early days of …
Global HIV Statistics
- As with the United States, there have been impressive declines in global HIV infections and deaths since 2004, when over 1.7 million deaths were reported. Today, the annual number of HIV-related deaths hover around 690,000—a reduction of roughly 60%.19 At the same time, there has been a leveling off of many of the early gains and an increase in infection rates in certain hotspots aro…