How long does it take monoclonal antibodies for migraines to start working? After first use, you might notice fewer migraine days within the first month. But healthcare providers try to give these medications about 3 to 6 months before deciding if they’re beneficial.
When to give monoclonal antibody treatment?
Note: Monoclonal antibody treatment needs to be given within 10 days of the start of symptoms. What to Expect During Monoclonal Antibody Treatment. Initially, health care workers within a hospital setting administered monoclonal antibodies with a one-time intravenous (IV) infusion, which takes anywhere from 30 minutes to an hour.
How long after monoclonal antibodies are you contagious?
Jan 06, 2022 · it has been 10 days or less since symptoms first started, and they have other health conditions that put them at higher risk. Monoclonal antibody treatment is most effective when given early—and the sooner it is given, the better. Treatment is not effective for people who are already hospitalized or severely ill with COVID-19.
How fast does monoclonal antibody treatment work?
May 12, 2021 · How Quickly Does Monoclonal Antibody Therapy Work? The infusion itself takes about 20 to 25 minutes, but before leaving, you must wait for an hour so the medical staff can observe you and ensure you don’t have an allergic reaction. They will also observe your symptoms to see if the illness is progressing or diminishing.
What to expect from monoclonal antibody treatment?
Feb 08, 2021 · Monoclonal antibody treatment for COVID-19 One of the most remarkable things about COVID-19 is how quickly physicians and scientists were able to respond and develop effective treatment for the disease in less than one year.

How do monoclonal antibodies work against COVID-19?
Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
How long could it take to develop antibodies against COVID-19?
It takes 5-10 days after you get infected to develop antibodies against the SARS-CoV-2 virus. Antibody tests could give people a false sense of security. They might go back to work and start to travel again when they could still catch or spread the virus.Jan 21, 2022
How long do COVID-19 antibodies last?
At this time, it is unknown for how long antibodies persist following infection and if the presence of antibodies confers protective immunity.Jan 31, 2022
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
Do people produce COVID-19 antibodies after infection?
Most people who've recovered from COVID-19 do make antibodies against the virus.Jan 21, 2022
How does the body develop immunity to COVID-19?
Once you've been exposed to a virus, your body makes memory cells. If you're exposed to that same virus again, these cells recognize it. They tell your immune system to make antibodies against it.Jan 21, 2022
How long does immunity last after the Pfizer COVID-19 vaccine?
Antibodies able to block the omicron coronavirus variant last four months after a third dose of Pfizer-BioNTech's vaccine, according to a study published Jan. 22 by bioRxiv.Jan 25, 2022
Do I need the COVID-19 vaccine if I still have antibodies?
Yes, the COVID-19 vaccines are recommended, even if you had COVID-19.Nov 23, 2021
Can you get reinfected with COVID-19?
Reinfections can and have happened even shortly after recovery, the researchers said. And they will become increasingly common as immunity wanes and new SARS-CoV-2 variants arise.Oct 19, 2021
What medication is not recommended before vaccinations for COVID-19?
It is not recommended you take over-the-counter medicine – such as ibuprofen, aspirin, or acetaminophen – before vaccination for the purpose of trying to prevent vaccine-related side effects. It is not known how these medications might affect how well the vaccine works.
Who should not take the Pfizer-BioNTech COVID-19 vaccine?
If you have had a severe allergic reaction to any ingredient in the Pfizer-BioNTech COVID-19 vaccine (such as polyethylene glycol), you should not get this vaccine. If you had a severe allergic reaction after getting a dose of the Pfizer-BioNTech COVID-19 vaccine, you should not get another dose of an mRNA vaccine.
What are the contraindications to the COVID-19 vaccine?
Contraindications to COVID-19 vaccination include: Severe allergic reaction (e.g., anaphylaxis) after a previous dose or to a component of the COVID-19 vaccine. Known diagnosed allergy to a component of the COVID-19 vaccine (see Appendix C for a list of vaccine components).
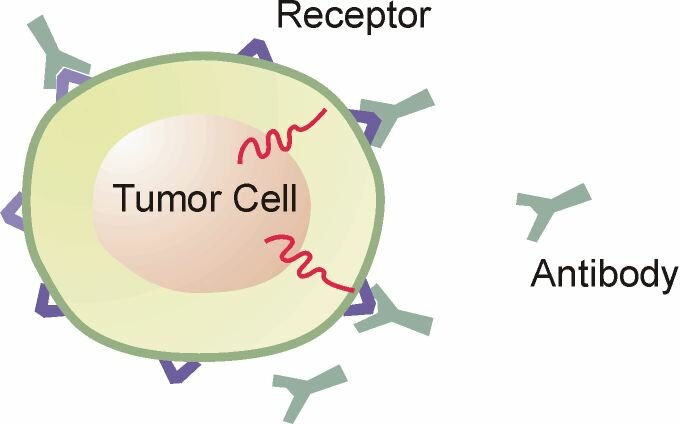
What is a monoclonal antibody?
Monoclonal antibodies are copies of human antibodies, created in a lab, that bolster your immune system to fight off an illness. With COVID-19, monoclonal antibodies bind to COVID-19’s spike protein to neutralize the virus and fight off the infection.
What are the requirements for a syringe?
The Food and Drug Administration (FDA) outlined specific guidelines of who qualifies for the treatment: 1 All adults ages 65 and older. 2 Anyone who is pregnant. 3 Children ages 12 to 17 with a body mass index (BMI) equal to or higher than 85% of children who are the same age and gender. 4 Adults ages 18 and older with a BMI of 25 or greater. 5 Anyone ages 12 and older with: diabetes, chronic kidney disease, a disease that weakens the immune system or a weakened immune system due to medication, cardiovascular disease (including congenital heart disease) or hypertension, chronic lung diseases, moderate to severe asthma, sickle cell disease, neurodevelopmental disorders (for example, cerebral palsy), genetic or metabolic syndromes and severe congenital anomalies, or regular use of medical technology (such as a feeding tube or a device that assists with breathing).
Is monoclonal antibody effective?
“This treatment is 70% effective in reducing rates of hospitalization and death, yet not many people know about it,” says Bruce Muma, M.D ., CEO of Henry Ford Physician Network.
What drugs are given in monoclonal infusions?
Those drugs given in the infusions are: bamlanivimab-etesevimab and casirivimab-imdevimab.
What are the conditions that affect the immune system?
Have underlying conditions, such as diabetes or chronic heart disease. Have a compromised immune system, such as, patients with cancer and those who have undergone transplantation. You are receiving high doses of steroids or other drugs to suppress your immune system.
What is the function of antibodies?
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
Does infusion cause nausea?
Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.