The protection from an antibody treatments doesn't last as long as a vaccine though. Typically the treatment would only provide protection for about a month. A vaccine takes a couple of weeks for the immune system to start providing protection, but monoclonal antibodies work right away.
Full Answer
When should you get an antibody test?
Jan 06, 2022 · it has been 10 days or less since symptoms first started, and they have other health conditions that put them at higher risk. Monoclonal antibody treatment is most effective when given early—and the sooner it is given, the better. Treatment is not effective for people who are already hospitalized or severely ill with COVID-19.
Do antibodies stay forever?
Note: Monoclonal antibody treatment needs to be given within 10 days of the start of symptoms. What to Expect During Monoclonal Antibody Treatment Initially, health care workers within a hospital setting administered monoclonal antibodies with a one-time intravenous (IV) infusion, which takes anywhere from 30 minutes to an hour.
How to know if you have antibodies?
Aug 25, 2021 · Monoclonal antibody treatment is generally given within 10 days of a positive COVID-19 test. “If the [monoclonal] antibodies are given relatively soon in high-risk patients, then [the treatment]...
Does natural immunity last longer?
Oct 07, 2021 · How long does it take to get monoclonal antibody infusion treatment? During the procedure, patients are seated in a comfortable chair, hooked up to an IV containing the antibody treatment, and ...
How long does it take to get monoclonal antibody infusion treatment?
During the procedure, patients are seated in a comfortable chair, hooked up to an IV containing the antibody treatment, and administered the drug cocktail intravenously for approximately 20 minutes.
Where can I find a monoclonal antibody infusion treatment center near me?
There are dozens of hospitals and healthcare providers in the Houston area offering monoclonal antibody infusions. KPRC 2 Investigates has a map below that can guide you to a provider near you. Just hover over one of the colored circles on the map to get the name and address of the provider nearest to you.
How long does it take for Bob to feel better after a blood test?
After the antibody infusion, Bob's symptoms continued to improve. Within several hours, Joyce began to feel much better, with no fever, chills or body aches. Lori says that their experience is consistent with other patients. "Most patients report improvement of symptoms with 24 to 48 hours after infusion," she says.
What is monoclonal antibody infusion?
The center has locations in Barron and Eau Claire. "A monoclonal antibody infusion is meant to boost your own body's immune system. These man-made antibodies are meant to mimic antibodies your immune system begins to make after being exposed to COVID-19," says Lori Arndt, a physician assistant in Infectious Diseases at Mayo Clinic Health System in ...
Why did the Wachsmuths get monoclonal antibodies?
The Wachsmuths qualified for the monoclonal antibodies due to age and other chronic health conditions that increased their chances of developing severe disease or requiring hospitalization. The day after their positive COVID-19 tests, Bob and Joyce received monoclonal antibody infusions at the same time in the same room at the clinic.
When will the Mayo Clinic open?
The Mayo Clinic COVID-19 Infusion Center opened in November 2020. The center has locations in Barron and Eau Claire.
Can family members receive infusions together?
Lori says it is not uncommon to have family members receive infusion treatments together. "We have had several family members come in together to receive treatment. It's a wonderful service to offer patients who may be feeling anxious or apprehensive about receiving treatment," says Lori.
What is the function of antibodies?
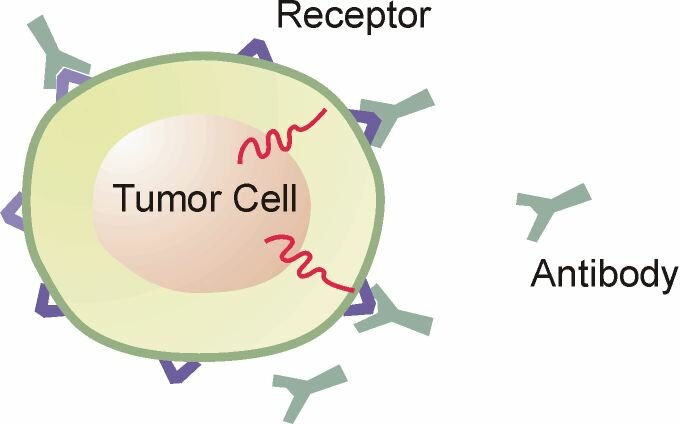
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
What antibody is used to block the virus?
Monoclonal antibodies against COVID-19 attach to the virus to block it from entering human cells. The monoclonal antibody protein also “marks” the virus to be broken down by the immune system and cleared from the body.
Can monoclonal antibodies cause nausea?
Most people tolerate monoclonal antibody infusions very well. Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.
When was monoclonal antibody first discovered?
It was discovered in the mid-1970s and brought to market in the mid-1990s. “Now, there are more than 60 FDA-approved monoclonal antibody treatments for various diseases, including autoimmune diseases, cancer, and other infections,” says Dr. Muma. “This type of treatment has been a huge breakthrough in healthcare.
What is a monoclonal antibody?
Monoclonal antibodies are copies of human antibodies, created in a lab, that bolster your immune system to fight off an illness. With COVID-19, monoclonal antibodies bind to COVID-19’s spike protein to neutralize the virus and fight off the infection.
What are the requirements for a syringe?
The Food and Drug Administration (FDA) outlined specific guidelines of who qualifies for the treatment: 1 All adults ages 65 and older. 2 Anyone who is pregnant. 3 Children ages 12 to 17 with a body mass index (BMI) equal to or higher than 85% of children who are the same age and gender. 4 Adults ages 18 and older with a BMI of 25 or greater. 5 Anyone ages 12 and older with: diabetes, chronic kidney disease, a disease that weakens the immune system or a weakened immune system due to medication, cardiovascular disease (including congenital heart disease) or hypertension, chronic lung diseases, moderate to severe asthma, sickle cell disease, neurodevelopmental disorders (for example, cerebral palsy), genetic or metabolic syndromes and severe congenital anomalies, or regular use of medical technology (such as a feeding tube or a device that assists with breathing).
Can you get monoclonal antibody therapy?
You cannot receive monoclonal antibody therapy if you have already progressed to severe illness—once you’re in the hospital or on oxygen, the treatment is not approved for use, so it’s incredibly important to talk to your doctor as soon as possible to see if you’d be a candidate. All adults ages 65 and older.
Who is Bruce Muma?
Bruce Muma, M.D., is an internal medicine physician with Henry Ford Health System. He is the CEO of Henry Ford Physician Network and is leading the expansion of the monoclonal antibody clinics at Henry Ford. Categories: FeelWell. Tags: Coronavirus.
Is monoclonal antibody effective?
“This treatment is 70% effective in reducing rates of hospitalization and death, yet not many people know about it,” says Bruce Muma, M.D ., CEO of Henry Ford Physician Network.
What is a monoclonal antibody?
Monoclonal antibodies are lab-made proteins, that can mimic the immune system's ability to fight off threats like the coronavirus.
Can they prevent Covid-19?
The antibody therapy made by Regneron is also authorized to be used as a preventative treatment, or what's known as a post-exposure prophylaxis.
Who can get monoclonal antibody treatments for Covid-19?
The treatments for people infected with Covid-19 are for non-hospitalized adults and pediatric patients 12 years of age and older who have a risk of getting severe Covid-19.
How does someone access the treatment?
The drugs don't come in a simple pill, so they wouldn't typically be available at the average doctor's office, but a doctor can prescribe them.
How effective are the treatments?
Studies show mAbs are highly effective at preventing high-risk patients from developing severe Covid-19 symptoms.
Are there side effects?
Allergic reactions are unlikely, but possible. Worsening symptoms after treatment can also happen, according to the FDA.
How much do the treatments cost?
The US has spent more than $2 billion on monoclonal antibody treatment doses. But as of now, the treatment is free to patients, although there may be an administration fee.
How early can you get tested for a drug?
We give these treatments to help keep you out of the hospitals and make the disease less severe. It is important to get tested as early as possible, within 10 days of showing symptoms.
What drugs are given in monoclonal infusions?
Those drugs given in the infusions are: bamlanivimab-etesevimab and casirivimab-imdevimab.
What are the conditions that affect the immune system?
Have underlying conditions, such as diabetes or chronic heart disease. Have a compromised immune system, such as, patients with cancer and those who have undergone transplantation. You are receiving high doses of steroids or other drugs to suppress your immune system.
Does a monoclonal antibody interfere with other medications?
Your kidneys or liver do not digest this drug, so it should not interfere with other medications you are on. Monoclonal antibodies attach to the spike protein of the SARS-CoV-2 virus (the virus that causes COVID-19). That keeps the virus from attaching itself to your cells.