Abstract Insulin stimulates cellular K+ uptake leading to hypokalemia. Cellular K+ uptake is accomplished by parallel stimulation of Na+/H+ exchange, Na+,K+,2Cl− co-transport, and Na+/K+ ATPase and leads to cell swelling, a prerequisite for several metabolic effects of the hormone. Little is known about underlying signaling.
What is hypokalemia and how can it be treated?
You are said to have hypokalemia if your potassium level is below 3.5 mmol/L. Mild hypokalemia can be managed with changes in diet. Severe hypokalemia occurs when your potassium level is below 2.5 mmol/L, which can be fatal and requires immediate medical attention.
Can insulin cause hypokalemia?
Trauma or insulin excess, especially if diabetic, can cause a shift of potassium into cells (hypokalemia). Potassium is excreted (or "flushed out" of your system) by your kidneys. Certain drugs or conditions may cause your kidneys to excrete excess potassium. This is the most common cause of hypokalemia.
Does insulin therapy for hyperkalemia cause hypoglycemia?
However, this therapy may be associated with significant hypoglycemia [ 14, 18 – 21 ]. In one study of hospitalized patients treated with IV insulin for hyperkalemia, 8.7% of the patients developed hypoglycemia (defined as blood glucose of <70 mg/dL [3.9 mmol/L]) [ 20 ].
What are the treatment options for hyperkalemia in hemodialysis patients?
Allon M, Copkney C. Albuterol and insulin for treatment of hyperkalemia in hemodialysis patients. Kidney Int. 1990;38(5):869–872.
See more
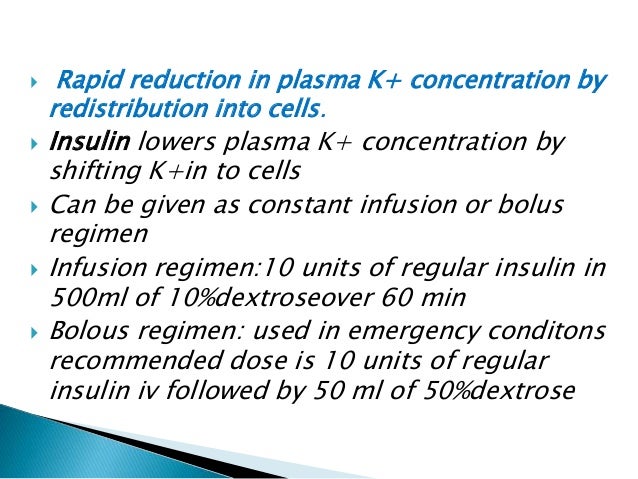
Why is insulin used to treat hyperkalemia?
Drugs used in the treatment of hyperkalemia include the following: Calcium (either gluconate or chloride): Reduces the risk of ventricular fibrillation caused by hyperkalemia. Insulin administered with glucose: Facilitates the uptake of glucose into the cell, which results in an intracellular shift of potassium.
What is the relationship between insulin and potassium?
If your potassium levels are too low, your body may make less insulin. That could lead to high blood sugar. Studies show that people with low potassium levels release less insulin, have higher blood sugar levels, and are more likely to get type 2 diabetes than those with normal potassium levels.
How does insulin stimulate the sodium potassium pump?
These results demonstrate that insulin induces vasodilation by stimulation of Na+,K+-ATPase. This activation of Na+,K+-ATPase could occur at the level of the endothelium rather than that of vascular smooth muscle and contributes to the endothelium-dependent vasodilator response to insulin.
How does insulin and glucose treat hyperkalemia?
Hyperkalemia is a life-threatening condition that requires prompt management in the ED. One of the most common treatment options is the administration of insulin and glucose to help shift potassium into the cell temporarily. Usually this is ordered as 10 units of regular insulin IV and 1 ampule of D50.
How does insulin and D50 lower potassium?
The rationale is based on the theory that exogenous glucose stimulates insulin secretion which shifts potassium into the cell. In a randomized, crossover study of 10 non-diabetic, ESRD patients on hemodialysis with hyperkalemia, dextrose alone led to a clinically significant decrease in serum potassium level.
How does insulin affect sodium?
The primary action of insulin on sodium balance is exerted on the kidney. Increases in plasma insulin concentration within the physiological range stimulate sodium reabsorption by the distal nephron segments and this effect is independent of changes in circulating metabolites or other hormones.
How does glucose affect potassium?
Potassium is generally stored in the fluid inside of the cells, but when there's too much glucose outside of the cells (blood sugar is too high), potassium moves outside of the cell, raising potassium levels in the blood.
Does hyperglycemia cause hypokalemia?
Hypokalemia is associated with impaired insulin secretion and decreased peripheral glucose utilization resulting in carbohydrate intolerance and hyperglycemia[47]. This is particularly problematic in diabetic patients causing a vicious circle where low serum K+ levels lead to poorly controlled DM and vice versa.
What is hypokalemia in blood?
What is Hypokalemia? Hypokalemia is defined as low potassium level in the blood. Potassium is an electrolyte whose concentration within the cells is higher than outside the cells i.e. in the blood. The potassium levels as measured in the laboratory indicate the blood levels of potassium, and not the levels within the cells. Normal potassium levels in the blood serum range from 3.5 to 5.0 mEq /l. Low blood potassium levels is referred to as hypokalemia, while high blood potassium levels are referred to as hyperkalemia. Hypokalemia can range from mild to severe. Mild - serum potassium level ranges from 3-3.5 mEq /L. Moderate - serum potassium level ranges between 2.5-3 mEq /L. Severe – serum potassium level is below 2.5 mEq /L Serum refers to the liquid portion of the blood that does not clot, which is used for measuring potassium levels. How are Potassium Levels Maintained at Normal Levels? Potassium is obtained from the diet and excreted through the kidneys. It is essential that potassium levels are tightly regulated by physiological mechanisms. The adrenal glands and the pancreas play an important role in maintaining blood potassium levels. The adrenal glands secrete a hormone called aldosterone, which increases excretion of potassium via the urine, while the pancreas secrete insulin, which drives potassium into body cells, thereby reducing its blood level. Alterations in serum potassium levels such as hypokalemia can be potentially life-threatening unless promptly addressed. Potassium is critical to the normal functioning of muscle and nerve cells. Hypokalemia therefore predominantly affects muscle and nerve function. What are the Causes of Hypokalemia? Hypokalemia may be caused by one or more of the following factors: Inadequate intake of potassium Excessive loss o Continue reading >>
What is the definition of hypokalemia?
Hypokalemia is serum potassium concentration < 3.5 mEq/L caused by a deficit in total body potassium stores or abnormal movement of potassium into cells. The most common causes are excess losses from the kidneys or GI tract. Clinical features include muscle weakness and polyuria; cardiac hyperexcitability may occur with severe hypokalemia. Diagnosis is by serum measurement. Treatment is giving potassium and managing the cause. Familial periodic paralysis is a rare autosomal dominant disorder characterized by transient episodes of profound hypokalemia thought to be due to sudden abnormal shifts of potassium into cells. Episodes frequently involve varying degrees of paralysis. They are typically precipitated by a large carbohydrate meal or strenuous exercise. Renal potassium losses Liddle syndrome is a rare autosomal dominant disorder characterized by severe hypertension and hypokalemia. Liddle syndrome is caused by unrestrained sodium reabsorption in the distal nephron due to one of several mutations found in genes encoding for epithelial sodium channel subunits. Inappropriately high reabsorption of sodium results in both hypertension and renal potassium wasting. Renal potassium wasting can also be caused by numerous congenital and acquired renal tubular diseases, such as the renal tubular acidoses and Fanconi syndrome, an unusual syndrome resulting in renal wasting of potassium, glucose, phosphate, uric acid, and amino acids. Hypomagnesemia is a common correlate of hypokalemia. Much of this correlation is attributable to common causes (ie, diuretics, diarrhea), but hypomagnesemia itself may also result in increased renal potassium losses. By inducing diarrhea, laxatives, especially when abused, can cause hypokalemia. Surreptitious diuretic or laxative use or both is a f Continue reading >>
What is a diabetic ketoacidosis?
Diabetic ketoacidosis (DKA) is a serious metabolic disorder that can occur in animals with diabetes mellitus (DM).1,2 Veterinary technicians play an integral role in managing and treating patients with this life-threatening condition. In addition to recognizing the clinical signs of this disorder and evaluating the patient's response to therapy, technicians should understand how this disorder occurs. DM is caused by a relative or absolute lack of insulin production by the pancreatic b-cells or by inactivity or loss of insulin receptors, which are usually found on membranes of skeletal muscle, fat, and liver cells.1,3 In dogs and cats, DM is classified as either insulin-dependent (the body is unable to produce sufficient insulin) or non-insulin-dependent (the body produces insulin, but the tissues in the body are resistant to the insulin).4 Most dogs and cats that develop DKA have an insulin deficiency. Insulin has many functions, including the enhancement of glucose uptake by the cells for energy.1 Without insulin, the cells cannot access glucose, thereby causing them to undergo starvation.2 The unused glucose remains in the circulation, resulting in hyperglycemia. To provide cells with an alternative energy source, the body breaks down adipocytes, releasing free fatty acids (FFAs) into the bloodstream. The liver subsequently converts FFAs to triglycerides and ketone bodies. These ketone bodies (i.e., acetone, acetoacetic acid, b-hydroxybutyric acid) can be used as energy by the tissues when there is a lack of glucose or nutritional intake.1,2 The breakdown of fat, combined with the body's inability to use glucose, causes many pets with diabetes to present with weight loss, despite having a ravenous appetite. If diabetes is undiagnosed or uncontrolled, a series of metab Continue reading >>
What is the importance of potassium in the body?
Physiology Potassium is the major intracellular cation (intracellular K+ concentration is approximately 140 mEq/L) and is important for maintaining resting membrane potential of cells, particularly muscle and nerves. 60-75% of total body potassium is found within muscle cells, with the remainder in bone. Only 5% of potassium is located in extracellular fluid (ECF), therefore potassium concentration in blood is not always a reflection of total body potassium levels. Plasma (ECF) K+ concentration is tightly regulated; fairly small changes can have marked effects on organ function, with severe abnormalities of plasma K+ being life-threatening situations. Plasma [K+] regulation Regulation of plasma K+ is mostly accomplished by renal excretion and movement of K+ from extracellular fluid to intracellular fluid (translocation). If these mechanisms are functioning normally, the amount of K+ ingested has little effect on plasma K+. Intake has less of an effect on plasma potassium levels, however, if one or more of the regulatory mechanisms is faulty, then the amount of K+ ingested can exacerbate abnormalities in plasma K+. In some species with high potassium diets (e.g. ruminants), changes in intake can affect plasma concentrations alone. Intake: Ingested K+ is absorbed non-selectively in the stomach and small intestine. If dietary K+ is deficient, renal excretion of K+decreases (but still occurs) but excretion can increase under states of chronic high K+ in the diet. Excretion: Potassium is excreted into the renal tubules and colon, with the latter contributing only a small amount to total K+ excretion. An additional source of potassium excretion is the saliva of ruminants. Urinary excretion of K+ occurs in the distal tubules. About 70% of filtered K+ is absorbed in the proxima Continue reading >>
How does potassium enter the body?
INTRODUCTION Hypokalemia is a common clinical problem. Potassium enters the body via oral intake or intravenous infusion, is largely stored in the cells, and then excreted in the urine. Thus, decreased intake, increased translocation into the cells, or, most often, increased losses in the urine, gastrointestinal tract, or sweat can lead to a reduction in the serum potassium concentration (table 1). This topic will review the major causes of hypokalemia. The evaluation and treatment of hypokalemia are discussed separately. (See "Evaluation of the adult patient with hypokalemia" and "Clinical manifestations and treatment of hypokalemia in adults".) DECREASED POTASSIUM INTAKE Potassium intake is normally 40 to 120 mEq per day, most of which is then excreted in the urine. The kidney is able to lower potassium excretion to a minimum of 5 to 25 mEq per day in the presence of potassium depletion [1]. Thus, decreased intake alone rarely causes significant hypokalemia. This was demonstrated in a study of normal individuals in whom lowering potassium intake to 20 mEq per day was associated with a reduction in serum potassium from 4.1 mEq/L at baseline to 3.5 mEq/L [2]. However, a low potassium intake can contribute to the severity of potassium depletion when another cause of hypokalemia is superimposed, such as diuretic therapy. INCREASED ENTRY INTO CELLS More than 98 percent of total body potassium is intracellular, chiefly in muscle [3,4]. The normal distribution of potassium between cells and the extracellular fluid is primarily maintained by the Na-K-ATPase pump in the cell membrane [3,4]. Increased activity of the Na-K-ATPase pump and/or alterations in other potassium transport pathways can result in transient hypokalemia due to increased potassium entry into cells. Continue reading >>
What is hypokalemia in the body?
What Is Hypokalemia? Hypokalemia is an electrolyte imbalance and is indicated by a low level of potassium in the blood. The normal adult value for potassium is 3.5-5.3 mEq/L. Potassium is one of many electrolytes in your body. It is found inside of cells. Normal levels of potassium are important for the maintenance of heart, and nervous system function. What Causes Hypokalemia? One way your body regulates blood potassium levels is by shifting potassium into and out of cells. When there is a breakdown or destruction of cells, the electrolyte potassium moves from inside of the cell to outside of the cell wall. This shift of potassium into the cells causes hypokalemia. Trauma or insulin excess, especially if diabetic, can cause a shift of potassium into cells (hypokalemia). Potassium is excreted (or "flushed out" of your system) by your kidneys. Certain drugs or conditions may cause your kidneys to excrete excess potassium. This is the most common cause of hypokalemia. Other causes of hypokalemia include: Increased excretion (or loss) of potassium from your body. Some medications may cause potassium loss which can lead to hypokalemia. Common medications include loop diuretics (such as Furosemide). Other drugs include steroids, licorice, sometimes aspirin, and certain antibiotics. Renal (kidney) dysfunction - your kidneys may not work well due to a condition called Renal Tubular Acidosis (RTA). Your kidneys will excrete too much potassium. Medications that cause RTA include Cisplatin and Amphotericin B. You may have hypokalemia from a loss of body fluids due to excessive vomiting, diarrhea, or sweating. Endocrine or hormonal problems (such as increased aldosterone levels) - aldosterone is a hormone that regulates potassium levels. Certain diseases of the endocrine system, s Continue reading >>
What hormones cause hypokalemia?
Certain hormones, particularly insulin, aldosterone, and sympathomimetics, are the most common cause of redistribution-induced hypokalemia. Insulin activates Na+ -K+ -ATPase, which results in active potassium uptake .
What is the normal level of potassium in the blood?
[1] Normal potassium levels are between 3.5 and 5.0 mmol/L (3.5 and 5.0 mEq/L) with levels below 3.5 mmol/L defined as hypokalemia. [1] [2] Mildly low levels do not typically cause symptoms. [3] Symptoms may include feeling tired, leg cramps, weakness, and constipation. [1] It increases the risk of an abnormal heart rhythm, which are often too slow, and can cause cardiac arrest. [1] [3] Causes of hypokalemia include diarrhea, medications like furosemide and steroids, dialysis, diabetes insipidus, hyperaldosteronism, hypomagnesemia, and not enough intake in the diet. [1] It is classified as severe when levels are less than 2.5 mmol/L. [1] Low levels can also be detected on an electrocardiogram (ECG). [1] Hyperkalemia refers to a high level of potassium in the blood serum. [1] The speed at which potassium should be replaced depends on whether or not there are symptoms or ECG changes. [1] Mildly low levels can be managed with changes in the diet. [3] Potassium supplements can be either taken by mouth or intravenously. [3] If given by intravenous, generally less than 20 mmol are given over an hour. [1] High concentration solutions (>40 mmol/L) should be given in a central line if possible. [3] Magnesium replacement may also be required. [1] Hypokalemia is one of the most common water–electrolyte imbalances. [4] It affects about 20% of people admitted to hospital. [4] The word "hypokalemia" is from hypo- means "under"; kalium meaning potassium, and -emia means "condition of the blood". [5] Play media Video explanation Signs and symptoms Mild hypokalemia is often without symptoms, although it may cause elevation of blood pressure, [6] and can provoke the development of an abnormal heart rhythm. Se Continue reading >>
What causes potassium to be pumped out of the body?
Trauma or insulin excess, especially if diabetic, can cause a shift of potassium into cells (hypokalemia). Potassium is excreted (or "flushed out" of your system) by your kidneys. Certain drugs or conditions may cause your kidneys to excrete excess potassium. This is the most common cause of hypokalemia.
How does insulin affect blood sugar?
Insulin has a number of actions on the body besides lowering your blood glucose levels. Insulin suppresses the breakdown and buildup of glycogen, which is the storage form of glucose, it blocks fat metabolism and the release of fatty acids, and it puts potassium into the cells by activating the sodium-potassium cellular channels. Insulin stimulates the uptake of glucose and potassium in all cells of the body but primarily fuels the muscle cells as well as some of the fat cells. In type 2 diabetes or metabolic syndrome (a form of metabolic disease), insulin is not functioning up to its normal level. The cells of the body become resistant to insulin and the blood sugar levels are elevated. The serum potassium (K+) level is a reflection of the total body stores of potassium, although it can be inaccurate in some conditions that affect the distribution of potassium in the body’s cells. The plasma potassium level determines the resting potential of the cells of the body. A person can have low potassium (hypokalemia) or high potassium (hyperkalemia), both of which are asymptomatic conditions that can be serious as they both cause heart arrhythmias. The Relationship between Insulin and Potassium Shortly after insulin was discovered, scientists revealed that insulin had something to do with the potassium levels in both the cells and in the blood. The insulin is the hormone in the body that keeps the potassium level in the blood within the normal range. When insulin is decreased, the potassium level rises and can rise even further if you eat something high in potassium, such as salt substitutes and bananas. When the potassium level is high, it causes the pancreas to release insulin in order to counteract the effects of high potassium levels. When you eat something that is high Continue reading >>
How does hyperkalemia affect the body?
How does hyperkalemia affect the body? Potassium is critical for the normal functioning of the muscles, heart, and nerves. It plays an important role in controlling activity of smooth muscle (such as the muscle found in the digestive tract) and skeletal muscle (muscles of the extremities and torso), as well as the muscles of the heart. It is also important for normal transmission of electrical signals throughout the nervous system within the body. Normal blood levels of potassium are critical for maintaining normal heart electrical rhythm. Both low blood potassium levels (hypokalemia) and high blood potassium levels (hyperkalemia) can lead to abnormal heart rhythms. The most important clinical effect of hyperkalemia is related to electrical rhythm of the heart. While mild hyperkalemia probably has a limited effect on the heart, moderate hyperkalemia can produce EKG changes (EKG is a reading of theelectrical activity of the heart muscles), and severe hyperkalemia can cause suppression of electrical activity of the heart and can cause the heart to stop beating. Another important effect of hyperkalemia is interference with functioning of the skeletal muscles. Hyperkalemic periodic paralysis is a rare inherited disorder in which patients can develop sudden onset of hyperkalemia which in turn causes muscle paralysis. The reason for the muscle paralysis is not clearly understood, but it is probably due to hyperkalemia suppressing the electrical activity of the muscle. Common electrolytes that are measured by doctors with blood testing include sodium, potassium, chloride, and bicarbonate. The functions and normal range values for these electrolytes are described below. Hypokalemia, or decreased potassium, can arise due to kidney diseases; excessive losses due to heavy sweating Continue reading >>
What are the etiological factors associated with hypokalemia?
Normal total body potassium with hypokalemia is a result of potassium redistribution from the extracellular to the intracellular space. Total body potassium depletion can result from either renal or extrarenal potassium losses. We suggest that the clinician evaluating a patient with hypokalemia consider four broad groups of etiologies: pseudohypokalemia, redistribution, extrarenal potassium loss, and renal potassium loss. Pseudohypokalemia Abnormal white blood cells, if present in large enough numbers, can take up extracellular potassium when stored for prolonged periods at room temperature, resulting in a low measured plasma potassium level. The apparent hypokalemia is an artifact of the storage procedure and is referred to as “pseudohypokalemia” . The most common underlying disease state is acute myelogenous leukemia. Rapid separation of the plasma or storing the sample at 4?C confirms the diagnosis, avoids this artifact, and prevents inappropriate treatment. Redistribution More than 98% of total body potassium is present in the intracellular fluid, predominantly in skeletal muscle cells, enabling small changes in the distribution of potassium to alter the extracellular concentration markedly. Certain hormones, particularly insulin, aldosterone, and sympathomimetics, are the most common cause of redistribution-induced hypokalemia. Insulin activates Na+ -K+ -ATPase, which results in active potassium uptake . Acute insulin administration produces rapid potassium shifts from the extra- to intracellular space, resulting in hyp Continue reading >>
What is hypokalemia in the body?
What Is Hypokalemia? Hypokalemia is an electrolyte imbalance and is indicated by a low level of potassium in the blood. The normal adult value for potassium is 3.5-5.3 mEq/L. Potassium is one of many electrolytes in your body. It is found inside of cells. Normal levels of potassium are important for the maintenance of heart, and nervous system function. What Causes Hypokalemia? One way your body regulates blood potassium levels is by shifting potassium into and out of cells. When there is a breakdown or destruction of cells, the electrolyte potassium moves from inside of the cell to outside of the cell wall. This shift of potassium into the cells causes hypokalemia. Trauma or insulin excess, especially if diabetic, can cause a shift of potassium into cells (hypokalemia). Potassium is excreted (or "flushed out" of your system) by your kidneys. Certain drugs or conditions may cause your kidneys to excrete excess potassium. This is the most common cause of hypokalemia. Other causes of hypokalemia include: Increased excretion (or loss) of potassium from your body. Some medications may cause potassium loss which can lead to hypokalemia. Common medications include loop diuretics (such as Furosemide). Other drugs include steroids, licorice, sometimes aspirin, and certain antibiotics. Renal (kidney) dysfunction - your kidneys may not work well due to a condition called Renal Tubular Acidosis (RTA). Your kidneys will excrete too much potassium. Medications that cause RTA include Cisplatin and Amphotericin B. You may have hypokalemia from a loss of body fluids due to excessive vomiting, diarrhea, or sweating. Endocrine or hormonal problems (such as increased aldosterone levels) - aldosterone is a hormone that regulates potassium levels. Certain diseases of the endocrine system, s Continue reading >>
What are the causes of hyperkalemia?
Hypokalemia and hyperkalemia are common electrolyte disorders caused by changes in potassium intake, altered excretion, or transcellular shifts. Diuretic use and gastrointestinal losses are common causes of hypokalemia, whereas kidney disease, hyperglycemia, and medication use are common causes of hyperkalemia. When severe, potassium disorders can lead to life-threatening cardiac conduction disturbances and neuromuscular dysfunction. Therefore, a first priority is determining the need for urgent treatment through a combination of history, physical examination, laboratory, and electrocardiography findings. Indications for urgent treatment include severe or symptomatic hypokalemia or hyperkalemia; abrupt changes in potassium levels; electrocardiography changes; or the presence of certain comorbid conditions. Hypokalemia is treated with oral or intravenous potassium. To prevent cardiac conduction disturbances, intravenous calcium is administered to patients with hyperkalemic electrocardiography changes. Insulin, usually with concomitant glucose, and albuterol are preferred to lower serum potassium levels in the acute setting; sodium polystyrene sulfonate is reserved for subacute treatment. For both disorders, it is important to consider potential causes of transcellular shifts because patients are at increased risk of rebound potassium disturbances. Potassium disorders are common. Hypokalemia (serum potassium level less than 3.6 mEq per L [3.6 mmol per L]) occurs in up to 21% of hospitalized patients and 2% to 3% of outpatients.1–3 Hyperkalemia (serum potassium level more than 5 mEq per L [5 mmol per L] in adults, more than 5.5 mEq per L [5.5 mmol per L] in children, and more than 6 mEq per L [6 mmol per L] in neonates) occurs in up to 10% of hospitalized patients and ap Continue reading >>
How does hyperkalemia affect the body?
How does hyperkalemia affect the body? Potassium is critical for the normal functioning of the muscles, heart, and nerves. It plays an important role in controlling activity of smooth muscle (such as the muscle found in the digestive tract) and skeletal muscle (muscles of the extremities and torso), as well as the muscles of the heart. It is also important for normal transmission of electrical signals throughout the nervous system within the body. Normal blood levels of potassium are critical for maintaining normal heart electrical rhythm. Both low blood potassium levels (hypokalemia) and high blood potassium levels (hyperkalemia) can lead to abnormal heart rhythms. The most important clinical effect of hyperkalemia is related to electrical rhythm of the heart. While mild hyperkalemia probably has a limited effect on the heart, moderate hyperkalemia can produce EKG changes (EKG is a reading of theelectrical activity of the heart muscles), and severe hyperkalemia can cause suppression of electrical activity of the heart and can cause the heart to stop beating. Another important effect of hyperkalemia is interference with functioning of the skeletal muscles. Hyperkalemic periodic paralysis is a rare inherited disorder in which patients can develop sudden onset of hyperkalemia which in turn causes muscle paralysis. The reason for the muscle paralysis is not clearly understood, but it is probably due to hyperkalemia suppressing the electrical activity of the muscle. Common electrolytes that are measured by doctors with blood testing include sodium, potassium, chloride, and bicarbonate. The functions and normal range values for these electrolytes are described below. Hypokalemia, or decreased potassium, can arise due to kidney diseases; excessive losses due to heavy sweating Continue reading >>
How does insulin affect blood sugar?
Insulin has a number of actions on the body besides lowering your blood glucose levels. Insulin suppresses the breakdown and buildup of glycogen, which is the storage form of glucose, it blocks fat metabolism and the release of fatty acids, and it puts potassium into the cells by activating the sodium-potassium cellular channels. Insulin stimulates the uptake of glucose and potassium in all cells of the body but primarily fuels the muscle cells as well as some of the fat cells. In type 2 diabetes or metabolic syndrome (a form of metabolic disease), insulin is not functioning up to its normal level. The cells of the body become resistant to insulin and the blood sugar levels are elevated. The serum potassium (K+) level is a reflection of the total body stores of potassium, although it can be inaccurate in some conditions that affect the distribution of potassium in the body’s cells. The plasma potassium level determines the resting potential of the cells of the body. A person can have low potassium (hypokalemia) or high potassium (hyperkalemia), both of which are asymptomatic conditions that can be serious as they both cause heart arrhythmias. The Relationship between Insulin and Potassium Shortly after insulin was discovered, scientists revealed that insulin had something to do with the potassium levels in both the cells and in the blood. The insulin is the hormone in the body that keeps the potassium level in the blood within the normal range. When insulin is decreased, the potassium level rises and can rise even further if you eat something high in potassium, such as salt substitutes and bananas. When the potassium level is high, it causes the pancreas to release insulin in order to counteract the effects of high potassium levels. When you eat something that is high Continue reading >>
What is DKA in diabetes?
Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus. [1] Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion, and occasionally loss of consciousness. [1] A person's breath may develop a specific smell. [1] Onset of symptoms is usually rapid. [1] In some cases people may not realize they previously had diabetes. [1] DKA happens most often in those with type 1 diabetes, but can also occur in those with other types of diabetes under certain circumstances. [1] Triggers may include infection, not taking insulin correctly, stroke, and certain medications such as steroids. [1] DKA results from a shortage of insulin; in response the body switches to burning fatty acids which produces acidic ketone bodies. [3] DKA is typically diagnosed when testing finds high blood sugar, low blood pH, and ketoacids in either the blood or urine. [1] The primary treatment of DKA is with intravenous fluids and insulin. [1] Depending on the severity, insulin may be given intravenously or by injection under the skin. [3] Usually potassium is also needed to prevent the development of low blood potassium. [1] Throughout treatment blood sugar and potassium levels should be regularly checked. [1] Antibiotics may be required in those with an underlying infection. [6] In those with severely low blood pH, sodium bicarbonate may be given; however, its use is of unclear benefit and typically not recommended. [1] [6] Rates of DKA vary around the world. [5] In the United Kingdom, about 4% of people with type 1 diabetes develop DKA each year, while in Malaysia the condition affects about 25% a year. [1] [5] DKA was first described in 1886 and, until the introduction of insulin therapy in the 1920s, it was almost univ Continue reading >>
How does insulin affect potassium levels?
Insulin shifts potassium into cells by stimulating the activity of Na+-H+antiporter on cell membrane, promoting the entry of sodium into cells, which lead s to activa tion of the Na+-K+ATPase , causing an electrogenic influx of potassium. IV insulin leads to a dose-dependent decline in serum potassium levels [16].
What is used to counter the adverse effects of hyperkalemia?
When dialysis is not immediately available, temporizing measures are employed. Intravenous calcium is used to counter the adverse myocardial effects of hyperkalemia but does not affect the serum concentration of potassium. Cation exchange resins are frequently used to increase colonic secretion of potassium.
Why is hypoglycemia lower in peritoneal dialysis?
Theoretically, the incidence of hypoglycemia is lower in peritoneal dialysis due to the presence of dextrose in the dialysis solution. The results from Apel's study emphasize the importance of intense blood glucose monitoring after insulin administration.
What are the risk factors for hypoglycemia?
Risk factors for hypoglycemia were: no prior diagnosis of DM, no use of DM medication prior to admission, and a lower pre-treatment glucose level. Hypoglycemia occurred at a median of 2 hours after insulin and persisted for a median of 2 hours.
What is the distribution of potassium between the intracellular and extracellular fluid compartments?
Distribution of potassium between the intracellular and the extracellular fluid compartments is regulated by physiologic factors such as insulin and catecholamines which stimulate the activity of the Na+- K+ATPas e. Only about 10% of the ingested potassium is excreted via the gut under normal physiologic conditions [1].
What is iatrogenic hypoglycemia?
The workgroup of the American Diabetes Association and the Endocrine Society defines iatrogenic hypoglycemia in patients with diabetes mellitus (DM) as “all episodes of an abnormally low plasma glucose concentration that expose the individual to potential harm.”.
How long does it take for potassium to shift to intracellular space?
Other measures that result in the shift of potassium from the extracellular to intracellular space, such as albuterol and insulin, have been proven to be effective in patients with chronic kidney disease (CKD) and are more rapid in onset, usually over 30–60 minutes [2, 12–14].
What are the four aims of hypokalemia?
The treatment of hypokalemia has four aims: (a) reduction of potassium losses, (b) replenishment of potassium stores, (c) evaluation for potential toxicities and (d) determination of the cause, in order to prevent future episodes, if possible.
What is hypokalemia in medical terms?
Hypokalemia is a common electrolyte disturbance, especially in hospitalized patients. It can have various causes, including endocrine ones. Sometimes, hypokalemia requires urgent medical attention. The aim of this review is to present updated information regarding: (1) the definition and prevalence of hypokalemia, ...
What are the effects of hypokalemia on the renal system?
The effects of hypokalemia regarding the renal function can be metabolic acidosis, rhabdomyolysis (in severe hypokalemia) and , rarely, impairment of tubular transport, chronic tubulointerstitial disease and cyst formation.
What is hypokalemia in the body?
Hypokalemia is present when serum levels of potassium are lower than normal. It is a rather common electrolyte disturbance, especially in hospitalized patients, with various causes and sometimes requires urgent medical attention (1). It usually results from increased potassium excretion or intracellular shift and less commonly from reduced ...
What happens if potassium is disrupted?
If potassium balance is disrupted (hypokalemia or hyperkalemia), this can also lead to disruption of heart electrical conduction, dysrhythmias and even sudden death. Potassium balance has a direct negative effect on (H+) balance at intracellular and extracellular level and the overall cellular activity. Balance of K+.
What is the pump of sodium?
K+is the main intracellular cation and almost all cells have the pump called ‘Na+-K+-ATPase’, which pumps sodium (Na+) out of the cell and K+into the cell leading to a K+gradient across the cell membrane (K+in > K+out), which is partially responsible for maintaining the potential difference across membrane.
