What is extubation? The removal of the Breathing Tube or Endotracheal Tube after Intubation
Tracheal intubation
Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate v…
What to expect after extubation?
after extubation can happen for many reasons such as a lung infection, decreased oxygen storage, acute. (sudden) swelling of the airway, injury to the airway, muscle weakness, abnormal reflexes of the airway. and/or the larynx. Other complications that can result after extubation includes spasms of the bronchi.
What is the difference between intubation and extubation?
is that intubation is (medicine) the introduction of a tube into an organ to keep it open, as into the larynx in croup while extubation is (medicine) the removal of a tube inserted by intubation. (medicine) The introduction of a tube into an organ to keep it open, as into the larynx in croup.
What is a good NIF for extubation?
What is a good NIF for extubation? Conclusions: In mechanically ventilated COPD patients with hypercapnic respiratory failure, the NIF threshold of ≤−25 cmH 2 O was a moderate-to-good predictor for successful ventilator liberation, and outperforms the traditional threshold of ≤−30 cmH 2 O.
Is positive pressure extubation a safe procedure?
There is no physiological rationale to support PEEP removal before extubation because existing data did not evidenced harmful effects with the use of moderate levels of PEEP. The use of positive pressure at extubation may also help prevent loss of aeration and pulmonary aspiration.
When should a patient be extubated?
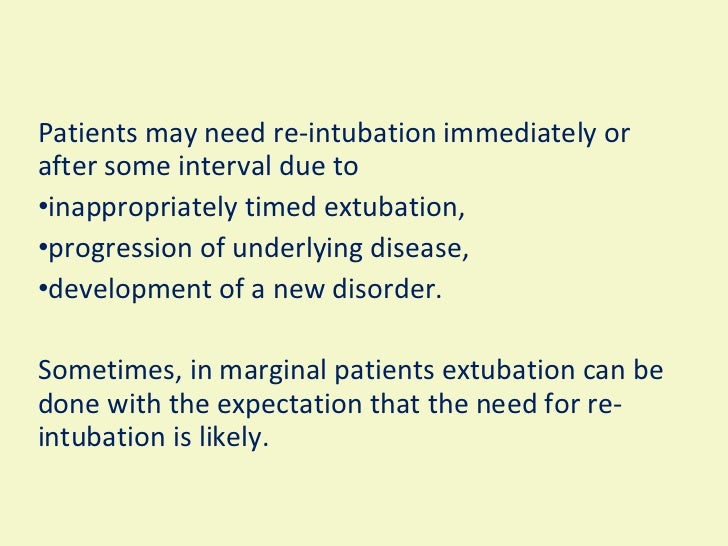
Extubation is usually decided after a weaning readiness test involving spontaneous breathing on a T-piece or low levels of ventilatory assist. Extubation failure occurs in 10 to 20% of patients and is associated with extremely poor outcomes, including high mortality rates of 25 to 50%.
How long is the extubation process?
Furthermore, studies have demonstrated that most SBT failures occur within 30 minutes,21,22 suggesting that a successful SBT of 30 minutes is as good an indicator of successful extubation as one of 120 minutes.
What is extubation procedure?
Extubation is the removal of an endotracheal tube (ETT), which is the last step in liberating a patient from the mechanical ventilator. To discuss the actual procedure of extubation, one also needs to understand how to assess readiness for weaning, and management before and after extubation.
What is the purpose of extubation?
Extubation refers to removal of the endotracheal tube (ETT). It is the final step in liberating a patient from mechanical ventilation.
How long can a person live after extubation?
On average, ICU patients survive between 35 minutes to 7.5 hours after terminal extubation.
Are patients awake during extubation?
Tracheal extubation can be performed while patients are awake or under deep anesthesia. Both techniques have their pros and cons. [1,2] Extubation in a light plane of anesthesia is the concern in awake extubation while leaving the patient with an unprotected airway is the reservation in deep extubation.
What happens when a patient is extubated?
Extubation is when the doctor takes out a tube that helps you breathe. Sometimes, because of illness, injury, or surgery, you need help to breathe. Your doctor or anesthesiologist (a doctor who puts you to “sleep” for surgery) puts a tube (endotracheal tube, or ETT) down your throat and into your windpipe.
Can you talk after extubation?
Problems speaking can persist for weeks or even months after intubation, but resting your voice will make no difference to recovery. Speech therapy, however, will teach you how to project your voice again and to be heard over background noise.
How long can a person be on a ventilator in an ICU?
Some people may need to be on a ventilator for a few hours, while others may require one, two, or three weeks. If a person needs to be on a ventilator for a longer period of time, a tracheostomy may be required.
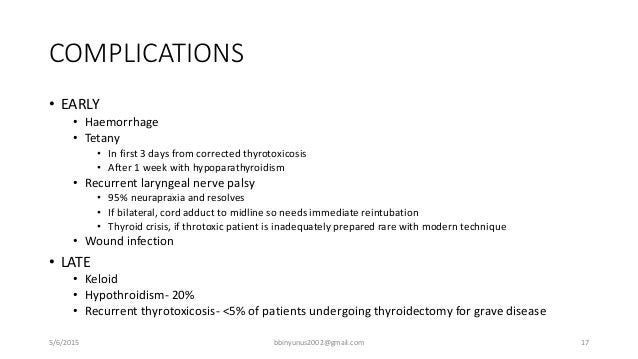
What is the most common complication after extubation?
The common complications immediately after extubation were coughing (6.6%) and oxygen desaturation (SaO2 < 90%) (2.4%), and in the recovery room, airway obstruction (3.8%) and coughing (3.1%).
What is extubation in medical?
Extubation is the removal of an endotracheal tube (ETT), which is the last step in liberating a patient from the mechanical ventilator. To discuss the actual procedure of extubation, one also needs to review how to assess readiness for weaning, and management before and after extubation. This activity reviews the overall process of extubation with special focus to the assessment of readiness, spontaneous breathing trial and few complications related to the process. The activity highlights the role of the interprofessional team including physicians, nurses and respiratory therapists in managing and improving care for all patients who undergo liberation from mechanical ventilation.
When does the preparation for extubation begin?
The preparation for extubation is a long process, which begins on the day of the patient's intubation and continues through the acute management of the primary problem which caused respiratory failure.
What is the difference between liberation and weaning?
Other terms related to extubation are 'weaning' and 'liberation.'. Weaning is a gradual transition from full invasive ventilatory support to spontaneous ventilation with minimal support. Liberation, on the other hand, means complete discontinuation of mechanical ventilation.
What is the last step in removing a patient from a ventilator?
Extubation is the removal of an endotracheal tube (ETT), which is the last step in liberating a patient from the mechanical ventilator. To discuss the actual procedure of extubation, one also needs to understand how to assess readiness for weaning, and management before and after extubation. Other terms related to extubation are 'weaning' ...
What is the last step in liberating a patient from the mechanical ventilator?
Extubation is the removal of an endotracheal tube (ETT), which is the last step in liberating a patient from the mechanical ventilator. To discuss the actual procedure of extubation, one also needs to understand how to assess readiness for weaning, and management before and after extubation.
What is the primary reason for intubation?
Any acute brain injury (including an invasive intracranial pressure measuring device for raised intracranial pressure), which was the primary reason for intubation.
What should be the mental status of a patient when extubated?
For most patients considered for extubation, mental status should be alert, awake, and able to follow commands - there should be no other neurologic abnormality impairing the patient's ability to breathe spontaneously.
What is extubation in intensive care?
What is extubation? The removal of the Breathing Tube or Endotracheal Tube after Intubation of the larynx or trachea (wind pipe). The purpose of extubation in Intensive Care is to take the Patient off mechanical ventilation ( Ventilators (Breathing Machines) so that he or she is able to breathe on their own.
Why is breathing difficult after extubation?
If your loved one has difficulties after being extubated, it usually comes down to a number of reasons such as. airway swelling. breathing muscle weakness. lung infection. Usually treatment of choice are.
How long does it take to get off a ventilator?
The weaning period can be relatively quick , within few hours after admission to Intensive Care or it can be very slow, sometimes over many days, depending on circumstances. Before extubation your loved one has been deemed ready for extubation by the doctor and the nurse. Other factors that need to be present before your loved one can be extubated are
How long does it take to wean someone from intensive care?
The weaning period can be relatively quick, within few hours after admission to Intensive Care or it can be very slow, sometimes over many days, depending on circumstances. Before extubation your loved one has been deemed ready for extubation by the doctor and the nurse.
What is the purpose of oxygen mask after extubation?
After extubation an oxygen mask will be applied to assist your loved one breathing spontaneously. Your loved one remains closely monitored ( Bedside Monitors) in order to manage a successful process after extubation.
What happens when you remove a breathing tube?
Usually what happens is that before the tube is removed, the nurse will suction down the breathing tube, in order to clear any sputum or secretions that may stop your loved one from breathing after extubation. Then another suction is required, this time in your loved ones mouth in order to clear any secretions there.
How long does it take for a tube to be removed?
Once the tube has been removed, the Patient may die quickly within minutes, but sometimes this may take hours to days. This will only be done after discussion with the Family and after views have been discussed of what is in the best interest of your loved one. This is done to enhance your loved ones dignity during this difficult time.
What is extubation in respiratory?
Extubation is performed with a sudden blockage of the endotracheal tube by foreign agents - for example, mucous and sputum secretions, foreign objects. After removal, reintubation or tracheostomy is performed, at the discretion of the doctor.
What is the protocol for extubation?
The clinical protocol for extubation should include careful monitoring of all vital signs and functions of a person after manipulation, rapid identification and response to respiratory disorders, if necessary, rapid reintubation or tracheostomy. [ 14]
Why is it difficult for my baby to breathe after extubation?
One of the complications of extubation can be laryngeal edema, which becomes a serious factor in the development of upper airway obstruction in young children: this manifests itself within six hours after the procedure. The supraglottic edema pushes the epiglottis backward, causing the glottis to block during inhalation. If there is retroaritenoidal edema behind the vocal cords, then this leads to a restriction of their abduction during inspiration. Subglottic edema narrows the cross-section of the laryngeal space. [ 20]
Why is the endotracheal tube removed?
The endotracheal tube is removed if there is no need to artificially maintain the patency of the airway. According to clinical characteristics, before extubation, the signs of the initial cause of respiratory failure should be mitigated, and the patient himself should have all the prerequisites for normal spontaneous respiration and gas exchange processes. [ 8]
What is the term for the introduction of a special tube inside the trachea?
Anesthesiologists often use concepts such as intubation and extubation . The first term - intubation - actually means the introduction of a special tube inside the trachea, which is necessary to ensure the patient's airway patency.
How long after extubation should you re-intubate?
First, you need to try to restore the patient's breathing using the Ambu bag, for 3-5 minutes. Only after normalization of the condition is it determined whether re-intubation is necessary. Reintubation is performed after preoxygenation. [ 7]
What is an indication for extubation?
Another indication for extubation can be considered a situation where the further presence of a tube in the trachea becomes impractical - for example, when it comes to the death of a patient. [ 3]