The removal of the Breathing Tube or Endotracheal Tube after Intubation
Tracheal intubation
Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate v…
Full Answer
What to expect after extubation?
after extubation can happen for many reasons such as a lung infection, decreased oxygen storage, acute. (sudden) swelling of the airway, injury to the airway, muscle weakness, abnormal reflexes of the airway. and/or the larynx. Other complications that can result after extubation includes spasms of the bronchi.
What is the difference between intubation and extubation?
is that intubation is (medicine) the introduction of a tube into an organ to keep it open, as into the larynx in croup while extubation is (medicine) the removal of a tube inserted by intubation. (medicine) The introduction of a tube into an organ to keep it open, as into the larynx in croup.
What is a good NIF for extubation?
What is a good NIF for extubation? Conclusions: In mechanically ventilated COPD patients with hypercapnic respiratory failure, the NIF threshold of ≤−25 cmH 2 O was a moderate-to-good predictor for successful ventilator liberation, and outperforms the traditional threshold of ≤−30 cmH 2 O.
Is positive pressure extubation a safe procedure?
There is no physiological rationale to support PEEP removal before extubation because existing data did not evidenced harmful effects with the use of moderate levels of PEEP. The use of positive pressure at extubation may also help prevent loss of aeration and pulmonary aspiration.
When should a patient be extubated?
Extubation is usually decided after a weaning readiness test involving spontaneous breathing on a T-piece or low levels of ventilatory assist. Extubation failure occurs in 10 to 20% of patients and is associated with extremely poor outcomes, including high mortality rates of 25 to 50%.
What is the purpose of extubation?
Extubation refers to removal of the endotracheal tube (ETT). It is the final step in liberating a patient from mechanical ventilation.
What are the steps to Extubate a patient?
0:598:04"Demonstration of Extubation Procedure" by Craig Smallwood ...YouTubeStart of suggested clipEnd of suggested clipWe're going to discuss with you today the process of assessing a patient and performing extubationMoreWe're going to discuss with you today the process of assessing a patient and performing extubation introduction extubation refers to the removal of the airway or the endotracheal tube from the patient
How long does it take to Extubate a patient?
Furthermore, studies have demonstrated that most SBT failures occur within 30 minutes,21,22 suggesting that a successful SBT of 30 minutes is as good an indicator of successful extubation as one of 120 minutes.
What happens when someone is Extubated?
Your doctor or anesthesiologist (a doctor who puts you to “sleep” for surgery) puts a tube (endotracheal tube, or ETT) down your throat and into your windpipe. This helps to get air into and out of your lungs. The process is called intubation. Extubation is taking that tube out.
What are the indications for extubation?
Indications. Endotracheal extubation is indicated when the clinical conditions that required airway protection with an endotracheal tube or that required mechanical ventilation are no longer present.
What is a one way extubation?
“Extubation” stands for removal of the breathing tube/endotracheal tube. A “one -way extubation”, simply describes the process of the breathing tube/endotracheal tube being removed when your loved one is approaching their end of life.
What is patient self extubation?
Self-extubation, defined as a deliberate action taken by the patient to remove the endotracheal tube, accounts for 68%-95% of all unplanned extubations.
What is the most common complication after extubation?
The common complications immediately after extubation were coughing (6.6%) and oxygen desaturation (SaO2 < 90%) (2.4%), and in the recovery room, airway obstruction (3.8%) and coughing (3.1%).
How long can a person live after extubation?
On average, ICU patients survive between 35 minutes to 7.5 hours after terminal extubation.
What are the steps a nurse must take after a patient is successfully extubated?
During extubation, the patient is encouraged to cough while the tube is being removed. Then, the patient will be encouraged to cough again, in order to promote mobilization of secretions. The patient should remain in a high-fowler position and immediately after extubation a supplement oxygen via mask will be provided.
Can you talk after extubation?
Problems speaking can persist for weeks or even months after intubation, but resting your voice will make no difference to recovery. Speech therapy, however, will teach you how to project your voice again and to be heard over background noise.
Why do you need an ETT tube?
The drugs that put you to sleep during surgery ( general anesthesia) may also hold down your breathing. That’s why you sometimes need the ETT in the first place. But the tube is uncomfortable, and you don't need it if you can breathe on your own. This typically happens as you start to wake up.
What is the process of getting air out of your lungs called?
This helps to get air into and out of your lungs. The process is called intubation. Extubation is taking that tube out.
How long does an ETT stay in place?
If you have an ETT because you're sick or hurt, it may be in place for as long as a couple of weeks. You may be awake as you use it.
Why can't you breathe on your own?
That’s because there can be serious results if you can’t breathe on your own, including brain damage and death.
What is extubation in intensive care?
What is extubation? The removal of the Breathing Tube or Endotracheal Tube after Intubation of the larynx or trachea (wind pipe). The purpose of extubation in Intensive Care is to take the Patient off mechanical ventilation ( Ventilators (Breathing Machines) so that he or she is able to breathe on their own.
Why is breathing difficult after extubation?
If your loved one has difficulties after being extubated, it usually comes down to a number of reasons such as. airway swelling. breathing muscle weakness. lung infection. Usually treatment of choice are.
What is the purpose of oxygen mask after extubation?
After extubation an oxygen mask will be applied to assist your loved one breathing spontaneously. Your loved one remains closely monitored ( Bedside Monitors) in order to manage a successful process after extubation.
What happens when you remove a breathing tube?
Usually what happens is that before the tube is removed, the nurse will suction down the breathing tube, in order to clear any sputum or secretions that may stop your loved one from breathing after extubation. Then another suction is required, this time in your loved ones mouth in order to clear any secretions there.
How long does it take for a patient to die after a tube is removed?
Once the tube has been removed, the Patient may die quickly within minutes, but sometimes this may take hours to days. This will only be done after discussion with the Family and after views have been discussed of what is in the best interest of your loved one.
How long does it take to wean someone from intensive care?
The weaning period can be relatively quick, within few hours after admission to Intensive Care or it can be very slow, sometimes over many days, depending on circumstances. Before extubation your loved one has been deemed ready for extubation by the doctor and the nurse.
What is the role of Mark in extubation?
Mark evaluates the physiology parameters for extubating the patient by assessing the patient's arterial blood gases (ABGs), oxygenation, ventilation, ventilatory mechanics , respiratory muscle strength , work of breathing, and ventilatory reserve.
Can you have ice chips after extubation?
It is common for patients to be hoarse post-extubation. This is a benign complication that can be managed with ice chips. The patient remains in the critical care unit for vital signs monitoring and management of any complications that may arise.
Why do I get laryngospasm after extubation?
[ 16] The most common cause of post-extubation laryngospasm is irritation with salivary secretions or blood, mainly with shallow anesthesia.
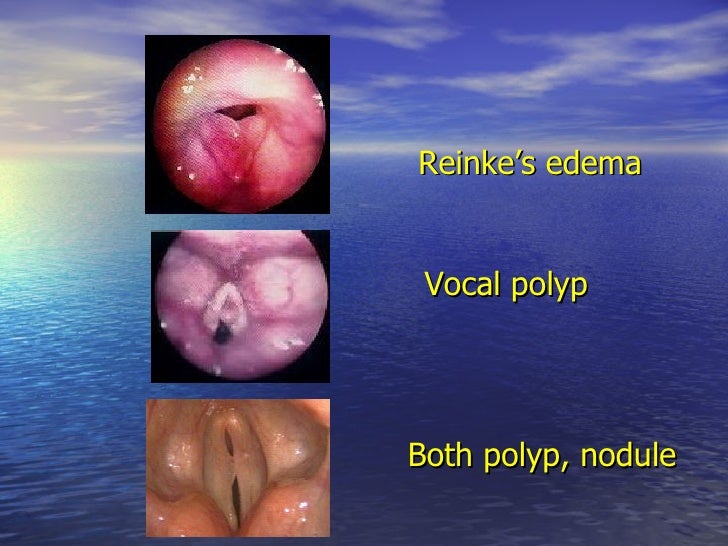
What is the most common cause of upper airway obstruction after extubation?
Laryngospasm is the most common cause of upper airway obstruction after extubation. The clinical picture of laryngospasm can be of varying severity and can be represented by both mild stridorious breathing and complete respiratory obstruction. Most often, the complication is found in childhood, against the background of surgical intervention on the organs of the respiratory system. [ 16]
When is the endotracheal tube removed?
In cases where there is no need to monitor the respiratory tract, the endotracheal tube, installed during intubation, is removed. This is usually done when a subjective and objective improvement in respiratory function is achieved. For a more comfortable and safe manipulation, the doctor must make sure that the patient can breathe on his own, that his respiratory tract is passable, and the tidal volume will be sufficient. In general, extubation is possible if the respiratory center is adequately able to initiate inspirations at normal frequency, depth, and rhythm. Additional conditions for the procedure are normal strength of the respiratory muscles, "working" cough reflex, high-quality nutritional status, adequate clearance of sedatives and muscle relaxants. [ 2]
Can extubation be fatal?
It is difficult to determine in advance the outcome of extubation, but it is necessary to take into account the fact that both premature and improperly performed manipulation can be fatal for the patient. The likelihood of developing certain consequences depends largely on the qualifications of the doctor, as well as on other background factors. Often, other pathologies in the patient's body, as well as secondary diseases, become the "culprits" of adverse consequences. [ 13]
Is it important to monitor after extubation?
Therefore, it is important to ensure maximum attention and monitoring of the patient's condition by the attending physician and anesthesiologist.
What medications should be given to terminal extubation?
Be aware of and closely monitor symptoms associated with the dying process. Appropriate medications such as opiates, benzodiazepines, and anticholinergics should be given early and as frequently as needed. Be familiar with the process of terminal extubation.
Why is withdrawal of life sustaining treatment delayed?
Withdrawal of life-sustaining treatment may be delayed in order to achieve appropriate and anticipatory symptom management. Delaying withdrawal of care for family arrival or spiritual rites should be considered by the provider but not unduly prolong suffering of the patient. Medications.
How to prevent hypoxia after extubation?
Following extubation, the conventional method of preventing hypoxia is application of controlled oxygen therapy (COT), usually via a facemask with the fraction of inspired oxygen targeted to a physiological parameter. Facemask oxygen, however, can be cumbersome and is associated with variable levels of oxygen delivery dependent upon the user’s peak inspiratory flow. In addition, mucosal drying may occur secondary to a lack of humidification, 52 increasing the risk of extubation failure secondary to secretion retention. High flow nasal oxygen therapy (HFNOT) is a relatively new development in adult populations offering humidified, warmed oxygen at flow rates ≤60 L/min. 53 This may be beneficial to recently extubated patients by providing more accurate oxygen concentrations, generating positive end expiratory pressure and improving gas exchange. 54
What is the process of weaning from IMV?
Guidance on the optimal strategies and timing of weaning are varied and the process is beset by potential complications. Extubation failure is arguably the most serious complication of weaning and is defined as the need for reintubation within a 48-hour period of initial removal of the patient from IMV. 1 Extubation failure is associated with several adverse healthcare-related outcomes and is thus of great significance to both healthcare providers and patients.
How long does it take for a SBT to fail?
Furthermore, studies have demonstrated that most SBT failures occur within 30 minutes, 21,22 suggesting that a successful SBT of 30 minutes is as good an indicator of successful extubation as one of 120 minutes.
Is extubation a challenge?
Despite many recent advances in ICU practice, optimal management of extubation remains a significant challenge to healthcare providers and carries a significant weight of morbidity and mortality should extubation failure occur. Several weaning strategies are well described in the literature, with an organised approach and consistency in practice seemingly more important than the weaning method used. Although a number of factors are described that may predict extubation failure, few of these are easily modifiable and no universal consensus exists to guide clinicians on when exactly to extubate.
laying the groundwork (1-2 days before extubation)
As the patient starts to approach extubation, the following factors should be optimized. Ideally, these should be considered as soon as the patient has stabilized on the ventilator: it's never too soon to start working towards extubation.
spontaneous breathing trial (SBT)
A spontaneous breathing trial should generally be performed daily among patients who are stable enough to undergo this. Rough (and largely arbitrary) criteria are listed below, but these need to be individualized.
if the patient fails the SBT
After failure, the patient should be placed back on a full level of ventilator support. The SBT may be repeated later in the day if there is something which can be easily manipulated which will improve the likelihood of success (e.g., holding sedation to allow the patient to wake up further). If there is no readily reversible cause of failure, it is usually best to repeat a SBT the following morning..
if the patient passes the SBT
If the patient passes a SBT, this suggests that they are strong enough to sustain the work of breathing. However, two other factors must also be considered: (#1) What is the risk of post-extubation laryngeal edema? (#2) Will the patient be able to maintain their airway?
post-extubation support
RCTs have demonstrated that extubation to HFNC reduces reintubation and ICU length of stay. The general concept is that HFNC reduces the work of breathing, thereby preventing patients from fatiguing after extubation.
timing of tracheostomy
For patients who are persistently unable to be extubated, tracheostomy should be considered (typically within a time frame of 1-2 weeks post intubation).
nocturnal extubation
It has been debated whether patients should be extubated at night, or whether extubation should be deferred to the following morning.