How does physician-patient communication affect outcomes?
Communication is an essential component of the medical care process, 8, 28 and through the therapeutic physician-patient relationship, patients are informed about their regimens, encouraged and supported in their motivation, and offered assistance in gathering and using needed resources to adhere. 29 Patient nonadherence continues to be a challenge for medical …
Why is it important to know the content of patient-care communication?
Results: Physician communication is significantly positively correlated with patient adherence; there is a 19% higher risk of non-adherence among patients whose physician communicates poorly than among patients whose physician communicates well. Training physicians in communication skills results in substantial and significant improvements in patient adherence …
How to improve communication in hospitals?
Physicians have been found to discourage patients from voicing their concerns and expectations as well as requests for more information.32 This negative influence of the doctors' behavior and the resultant nature of the doctor-patient communication deterred patients from asserting their need for information and explanations.32 Patients can feel disempowered and may be unable …
What are the effects of poor communication in healthcare?
Aug 01, 2009 · The way a physician communicates with his or her patient affects outcome of care, including patient satisfaction, health status, recall of information and adherence. The authors consider the results of certain research studies between 1949 and 2008 to see if there is an overall positive correlation between physician communication and patient adherence.

How does communication affect patient care?
What are the factors that can affect patient practitioner communication?
Why is it important to communicate effectively with patients?
What are the factors affecting the interaction between the patient and the physician?
Which are the barriers in doctor/patient relationship?
What are the benefits of effective communication in healthcare?
- Improved Patient-Provider Interactions. ...
- Improved Patient Satisfaction. ...
- Decrease Patient Complaints & Readmissions. ...
- Improve Internal Teamwork & Collaboration.
Why is communication important in healthcare teams?
Why is communication in nursing Important?
Why is communication important in medical care?
Conclusion: Communication in medical care is highly correlated with better patient adherence, and training physicians to communicate better enhances their patients' adherence. Findings can contribute to medical education and to interventions to improve adherence, supporting arguments that communication is important and resources devoted to improving it are worth investing in. Communication is thus an important factor over which physicians have some control in helping their patients to adhere.
Is physician communication positively correlated with patient adherence?
Results: Physician communication is significantly positively correlated with patient adherence; there is a 19% higher risk of non-adherence among patients whose physician communicates poorly than among patients whose physician communicates well. Training physicians in communication skills results in substantial and significant improvements in ...
How does effective doctor-patient communication help?
In addition to minimizing avoidance behavior, which prevents patients from expressing opinions, effective doctor-patient communication should involve productive conversation, which involves understanding of both parties' perspectives, by shifting from a perspective that is rigidly certain of one's belief to a more exploratory approach that strives to understand the situation from another perspective.41 Recognizing the impact of patient reciprocation of communication and affect in a medical visit is important as it may help create positive exchanges to defuse negative patterns.25
What is the purpose of effective communication between doctors and patients?
Effective doctor-patient communication is a central clinical function, and the resultant communication is the heart and art of medicine and a central component in the delivery of health care.7,8,16The 3 main goals of current doctor-patient communication are creating a good interpersonal relationship, facilita ting exchange of information , and including patients in decision making.4,7,11,17Effective doctor-patient communication is determined by the doctors' “bedside manner,” which patients judge as a major indicator of their doctors' general competence.1
What is the purpose of patient-patient communication?
Patients construct their own version of adherence according to their personal world views and social contexts, which can result in a divergent expectation of adherence practice.9,13,15Good doctor-patient communication is a mechanism used to gain an understanding of patients' social context, expectations, and experience.9,13,42With collaborative communication, a particular condition, perspective, or fact can be identified, allowing for a view from a different perspective, drawing attention for a better assessment and the subsequent treatment.41In this model, effective doctors acknowledge and respect patients' rights to make decisions and choices.13
Why do doctors avoid discussing patients' problems?
There are reported observations of doctors avoiding discussion of the emotional and social impact of patients' problems because it distressed them when they could not handle these issues or they did not have the time to do so adequately. This situation negatively affected doctors emotionally and tended to increase patients' distress.26This avoidance behavior may result in patients being unwilling to disclose problems, which could delay and adversely impact their recovery.26
What are some examples of influences that a patient takes into account on the doctor's advice?
Example of influences that a patient takes into account on the doctor's advice. STRATEGIES FOR IMPROVEMENT. Communication Skills. Communication skills involve both style and content.36Attentive listening skills, empathy, and use of open-ended questions are some examples of skillful communication.
Why do medical students lose communication skills?
It has been observed that communication skills tend to decline as medical students progress through their medical education, and over time doctors in training tend to lose their focus on holistic patient care.32Furthermore, the emotional and physical brutality of medical training, particularly during internship and residency, suppresses empathy, substitutes techniques and procedures for talk, and may even result in derision of patients.32
How do beliefs affect patients?
Beliefs and values affect the doctor-patient relationship and interaction.9Divergent beliefs can affect health care through competing therapies, fear of the health care system, or distrust of prescribed therapies.37This perception gap may negatively affect treatment decisions and therefore may influence patient outcomes despite appropriate therapy.17Although doctors use a biomedical model to understand illness, patient beliefs and values are influenced by social and behavioral factors as well as biology or anatomy.17
What is the importance of communication skills in a physician?
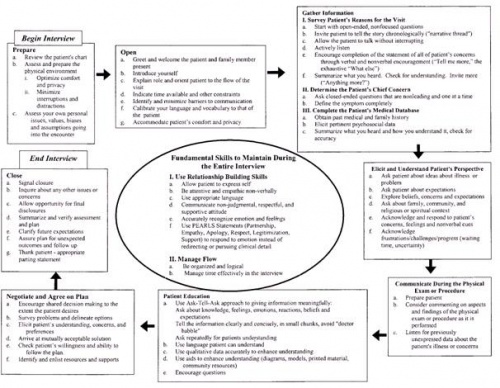
Physicians’ ability to effectively and compassionately communicate information is key to a successful patient–physician relationship. The Accreditation Council for Graduate Medical Education identified interpersonal and communication skills as one of six areas in which physicians-in-training need to demonstrate competence 1. This Committee Opinion reviews interviewing techniques to help the busy obstetrician–gynecologist effectively obtain a complete medical history, and discusses communication skills to assist in effectively relaying treatment plans.
Why is it important for physicians to communicate information?
ABSTRACT: Physicians’ ability to effectively and compassionately communicate information is key to a successful patient–physician relationship. The current health care environment demands increasing clinical productivity and affords less time with each patient, which can impede effective patient–physician communication.
What is shared decision making?
An extension of the partnership model is the concept of shared decision making, which is defined as a process where both patients and physicians share information, express treatment preferences, and agree on a treatment plan 13. The process is applicable if two or more reasonable medical options exist 14. The physician shares with the patient the relevant risk and benefit information on all reasonable treatment alternatives and the patient shares with the physician all relevant personal information that might make one treatment more or less tolerable than others 15. This paradigm of communication may be a marked departure from the traditional doctor-centered model. An example of shared decision making is that of the National Institutes of Health Consensus Panel on vaginal birth after cesarean delivery 16. The Consensus Panel recommended that the decision for vaginal birth after cesarean delivery or repeat cesarean delivery should occur only after a conversation between the patient and her physician, incorporating the risks and benefits and the patient’s preferences. Shared decision making can increase patient engagement and reduce risk with resultant improved outcomes, satisfaction, and treatment adherence 17.
How to encourage patients to write down their questions?
Encourage patients to write down their questions in preparation for appointments. A form for writing down questions can be given to patients on their arrival at the office. An organized list of questions can facilitate conversation on topics important to the patient.
What does "reassure the patient" mean?
Reassure the patient you are and will be available to help.
How does the Health Insurance Portability and Accountability Act protect privacy?
Further, while the Privacy Rule does not prohibit the use of unencrypted e-mail for treatment-related communication between health care providers and patients, other safeguards should be applied to reasonably protect privacy , such as limiting the amount or type of information disclosed through unencrypted e-mail 19. The physician time spent answering and managing e-mail should be acknowledged, and efforts should be made to advocate for compensation for additional time spent by physicians and staff to provide this service. When the patient has a complicated question or issues or has questions regarding symptoms, face-to-face contact between the physician and the patient may be preferable.
Why is increased time for visits important?
Increased time for visits is crucial in efforts to improve patient-centered interviewing, shared decision making, and improved patient–physician communication.
How to communicate with a patient?
Engage face to face. The way you position yourself in relation to your patient can also help convey that you're listening and concerned about what the patient has to say. Position yourself so that you can speak with the patient face to face and make eye contact.
Why is communication important in medical school?
Effective communication is one of the most important skills you can develop during the course of your medical training. Building rapport with your patients is the starting point for developing mutual respect and trust, which is vital to the therapeutic relationship.
Why do doctors sit down?
One of the most common complaints patients have about doctors is that they seem rushed. Much of the time, your day is going to be packed and fast-paced. However, the simple act of sitting down rather than standing to talk to your patient can make them feel more at ease and more willing to engage with you in a meaningful way. Given how hectic most physicians' schedules are, it's worth a deliberate reminder to use your body language to show you're slowing down for your patients and giving them your undivided attention.
How does body language affect doctors?
Body language not only indicates how doctors feel — consciously or not — about their patients, but can also impact how patients perceive their physicians. An article in Anesthesiology found that actor anesthesiologists who presented with "confident, high-power poses" were perceived as more intelligent and better at their jobs. Patients preferred these anesthesiologists to those with low-power postures.
How do nonverbal cues affect patient trust?
Nonverbal cues can affect rapport, patient trust, the willingness of the patient to adhere to the plan of care and the patient's satisfaction with the doctor-patient relationship. The study analyzed and scored doctors' communication with white versus black patients.
How does positive body language help patients?
In short, while it may take a conscious effort at first, using positive body language can help strengthen your patient interactions. Once you fall into these habits, you may notice your patients are more open with you and more receptive to your advice.
How to be more communicative?
2. Be conscious of your arms and shoulders. Be aware of the positions of your arms and shoulders, as these body parts are particularly communicative, whether you intend them to be or not. Avoid a posture where your arms are crossed or your shoulders are raised.
How does physician-patient communication affect health outcomes?
Effective physician-patient communication has been shown to positively influence health outcomes by increasing patient satisfaction, leading to greater patient understanding of health problems and treatments available, contributing to better adherence to treatment plans, and providing support and reassurance to patients.
Why is it important to communicate with patients?
In addition to having effective communication, it is important that medical decisions stem from a collaborative process between physicians and patients. Decision makingis a process in which patients should be involved from the very beginning, and the result is a decision which reflects the physician’s medical knowledge as well as the patient’s values and beliefs. iv Collaborative communication and decision making have been correlated with greater patient satisfaction and loyalty. Working from a collaborative framework along with effective physician-patient communication can also strengthen a physician’s ability to utilize a personalized health care model through patientempowerment. v
What is trust in a physician?
Trust is a fundamental characteristic of the physician-patient relationship. Patients must trust that their physicians will work in their best interests to achieve optimal health outcomes. Patients’ trust in their physicians has been demonstrated to be more important than treatment satisfactionin predictions of patient adherence to recommendations and their overall satisfaction with care. i Studies have also shown that trust is additionally a strong predictor of a patient continuing with their provider. ii Trust extends to many different aspects of the physician-relationships including, but not limited to: physicians’ willingness to listen to patients, patients’ believing that physicians value patient autonomy and ability to make informed decisions, and patients feeling comfortable enough to express and engage in dialogue related to their health concerns.
What is the dynamic between physicians and patients?
The dynamic between physicians and patients refers to the communication patterns and the extent to which decision making is shared between ...
What is the goal of a physician-patient relationship?
Ultimately, the overarching goal of the physician-patient relationship is to improve patient health outcomes and their medical care. Stronger physician-patient relationships are correlated with improved patient outcomes.
Is physician-patient communication a core element of quality?
The idea of viewing physician-patient relationships as a core element of quality health care is not something new, however understanding and assessing the factors that influence this relationship is just beginning. Effective physician-patient communication has been shown to positively influence health outcomes by increasing patient satisfaction, ...
Why is communication important in health care?
The purpose of this study was to measure the content and prevalence of verbal and nonverbal communications between physical therapists and patients with back pain.
How to measure communication between physical therapist and patient?
To measure communication, it is necessary to directly observe the interaction taking place between the physical therapist and the patient. 26 This interaction can be recorded with either videotapes or audiotapes, although videotape recording has the advantage of being able to record nonverbal communication in addition to verbal utterances. Conversely, recording patients in a state of undress may deter potential participants and could raise ethical issues. For the purposes of this study, recording nonverbal communication was a priority; therefore, with express (written) consent from both parties, the interaction between the physical therapist and the patient was recorded with videotape during the first treatment session following the initial assessment. This session was chosen because it was a less structured encounter than the initial assessment but was still early enough in the patient's treatment to capture the developing therapeutic relationship.
Why are affective behaviors important for physical therapy?
Previous research showed that considerable affective behaviors are required for an effective interaction between a physical therapist and a patient. 30 In the present study, these behaviors were shown to be less common than content behaviors; a possible explanation is that a considerable amount of advice still was being imparted to the patients during the early sessions. It is possible that affective behaviors become more prevalent in subsequent sessions, when the therapeutic relationship is more established; this issue is worthy of further research. A more likely reason for the underrepresentation of empathic behaviors in the present study, however, was the presence of the video camera, as the therapists reported that this decreased the amount of nonclinical communication that occurred. This potential limitation also was identified in previous studies. 31,32 It is not known from the present study what influence the camera was perceived to have on the patients’ communication, as this factor was not measured; this issue is worthy of further research.
What is nonverbal communication?
3 The effectiveness of any verbal message conveyed to another individual relies on his or her ability to listen, hear, and assimilate the message appropriately. 4 Nonverbal communication includes all behaviors that convey messages without the use of verbal language. 5 Attempts have been made to quantify the relative importance of verbal and nonverbal behaviors, with estimates of the nonverbal component comprising 55% to 97%, 6 90%, 7 and 93% 8 of the message. Despite the variations in these values, nonverbal aspects of communication are consistently thought to be more influential than verbal behaviors. According to Waddell, 9 when the nonverbal message conflicts with the verbal message, people probably will not believe what is said.
How many verbal statements are made by physical therapists?
A total of 2,055 verbal statements were made. Physical therapists spent approximately twice as much time talking as patients, with content behaviors (such as taking history and giving advice) comprising 52% of verbal communications.
What is the gold standard instrument for measuring communication?
Despite the importance of communication, there is no gold standard instrument for meas uring communication, and various methods have been used within the health care fields; qualitative methods have been used to determine health care professionals’ and patients’ opinions of what constitutes an effective interaction, 23 and quantitative methods have been used to measure verbal and nonverbal communications with an array of classification schemes. Although these methods have resulted in greater insight into styles of communication, relatively little still is known about the content of health care consultations. 24 To date, this work generally has focused on doctor-patient interactions and has been reported less widely in other health care professions.
How is the prevalence of communication measured?
The prevalence and content of communication can be measured with video analysis and validated tools. Communication is an extremely important but underexplored dimension of the patient-therapist relationship, and the methods described here could provide a useful model for further research and reflective practice.
How does communication affect patient satisfaction?
Communication failures often have a negative effect on patient and staff satisfaction. Effective communication will: Improve quality of care and patient outcomes. Enhance the patient experience. Improve patient satisfaction scores. Reduce the cost of healthcare. Reduce stress for clinicians and prevent burnout.
Why do hospitals have communication problems?
Communication problems occur for a variety of reasons such as ineffective policies and procedures, language difficulties, poor communication skills, workload pressure, EHR issues, poor documentation, conflicts between staff members, and ineffective communication systems in hospitals.
What is poor communication?
Poor communication between clinicians and patients can result in misunderstandings about medications and the miscommunication of follow up instructions, which can result in poor outcomes and readmissions, and could result in a patient coming to harm. Poor communication can also result in inadequate informed consent, ...
What are the most common communication failures between clinicians?
The most common communication failures between clinicians involve the miscommunication of important information about a patient’s symptoms or condition and poor documentation of patient information. These issues can lead to incorrect decisions being made about treatment and delays to treatment when the severity of the patient’s condition is not understood.
How does poor communication affect healthcare?
The effects of poor communication in healthcare can have extremely serious consequences. As with other businesses, poor communication decreases profits but in healthcare communication failures negatively affect patient outcomes. Poor communication results in misdiagnoses and other medical mistakes that can easily lead to avoidable health ...
What are the communication strategies in hospitals?
These include the RELATE model (Reassure, Explain, Listen/answer questions, Take action, Express appreciation), the STICC Protocol (Situation, Task, Intent, Concern, calibrate), and the BATHE Protocol (Background, Affect, Troubles, Handling, Empathy). See Communication Strategies in Healthcare.
Why are there delays in hospitals?
Patients often experience long delays, often at several stages of their journey in a hospital. Many of the delays are the result of poor communication between staff. These communication issues slow patient throughput, increase hospital stays, and are a key factor in poor patient satisfaction scores and are costly for hospitals.
