Health insurers ration your care by limiting the practitioners you may visit because they negotiate fees with those healthcare providers. They will only pay for you to visit the ones they have negotiated the lowest fees with. 3 Health insurers ration care through co-pays, deductibles, and caps.
Full Answer
How is health care rationed in the United States?
Examples of how health care is rationed in the U.S. by limiting access to certain types of care or providers include: Pre-authorization requirements. In this case, your health insurer will refuse to pay for non-emergency health care if you didn’t get the health insurer’s permission before getting the care.
What are the two forms of rationing in healthcare?
Instead, U.S. healthcare rationing is more subtle and usually presents in one of two forms: 1 Limiting access to certain types of health care or healthcare providers. 2 Increasing barriers to health care in order to discourage frivolous use, expensive care when a less expensive... More ...
How does Medicare pay for inpatient rehab?
You must receive care at a Medicare-approved facility or from a Medicare-approved provider. Your provider must set up a plan of care. Part A helps with payment for inpatient treatment at a hospital or inpatient rehab center. Part B helps with payment for outpatient treatment services through a clinic or a hospital outpatient center.
Do health insurers ration care?
Health insurers ration care, but they don't call it rationing, and they don't even want you to realize that it is rationing. This is referred to as "covert rationing" or "implicit rationing."

How is healthcare rationed in the United States?
In the public sector, primarily Medicare, Medicaid and hospital emergency rooms, health care is rationed by long waits, high patient copayment requirements, low payments to doctors that discourage some from serving public patients and limits on payments to hospitals."
What is the Medicare approved amount for radiation treatments?
The deductible amount for Medicare Part A is $1,408 per benefit period in 2020.
Does Medicare cover stereotactic radiosurgery?
CMS Publication 100-03, Medicare National Coverage Determinations Manual, Chapter 1, Part 2: Section 160.4 Stereotactic cingulotomy as a means of psychotherapy is investigational and non-covered.
What is rationing health care based off of?
We proposed a model of rationing in health systems based on the system theory (Fig. 2). The health services rationing system is concerned with deciding which goods or services must be restricted and which patients should be given limited access to such services.
Does Medicare pay for chemotherapy and radiation?
Medicare covers chemotherapy if you have cancer. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers it if you're a hospital inpatient. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What is the average cost of radiation treatment?
For patients not covered by health insurance, radiation therapy can cost $10,000-$50,000 or more, depending on the type of cancer, number of treatments needed and especially the type of radiation used.
How Much Does Medicare pay for CyberKnife?
The average cost to Medicare for CyberKnife prostate cancer treatment is $29,000, Saul reported.
Is radiotherapy covered by Medicare?
Your total cost of radiotherapy treatment is largely covered through Medicare via the Medicare Benefits Scheme and the Extended Medicare Safety Net programs and we can provide you with a guideline of what you are likely to pay out-of-pocket after your treatment plan has been confirmed.
Does Medicare cover palliative radiation?
One of the biggest obstacles to palliative radiotherapy is Medicare reimbursement. Hospice benefits cover the service but do not pay the actual cost of the service.
Is rationing healthcare good?
Is healthcare rationing good? In some ways, yes. Rationing care helps us to use our limited resources more wisely, picking and choosing among options and trying to get only the care that's truly necessary.
Why should we ration healthcare?
If the U.S. system spent less on expensive treatments for those who, with or without the drugs, have at most a few months to live, it would be better able to save the lives of more people who, if they get the treatment they need, might live for several decades.
Why do we ration?
Rationing is the allocation of scarce resources, which in health care necessarily entails withholding potentially beneficial treatments from some individuals. Rationing is unavoidable because need is limitless and resources are not.
How much is Medicare Part A 2020?
The deductible amount for Medicare Part A is $1,408 per benefit period in 2020. A benefit period starts the day after you’re admitted to a hospital. It ends after you haven’t had any inpatient care for 60 days following that hospital stay. You may have more than one benefit period within a calendar year.
What is Medicare Part B?
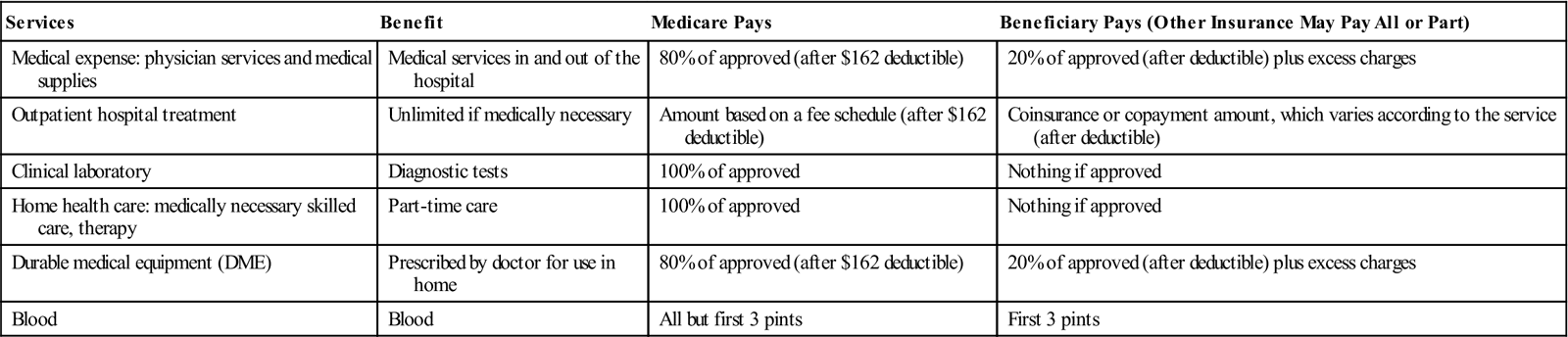
Medicare Part B. Your Medicare Part B plan covers costs for cancer treatments and visits at outpatient medical centers like doctors’ offices and freestanding clinics. Services and treatments for cancer that may be covered under Part B include: cancer screening and prevention services. radiation therapy. medications to manage side effects ...
How does radiation therapy work?
Radiation therapy involves using high-intensity beams of energy to destroy cancer cells by destroying their DNA. This then prevents them from multiplying and traveling throughout the body. There are two types of radiation therapy: external beam and internal. Here’s how they work: External beam radiation.
What is Medicare Supplemental Insurance?
Medigap (Medicare supplemental insurance) is a type of private insurance plan that helps cover your share of Medicare costs if you have parts A and B. Parts A and B together are known as original Medicare.
How much is the maximum out of pocket for a coinsurance plan?
Many plans have 20 percent coinsurance costs until you reach the out-of-pocket maximum (the highest possible is $6,700 ). After you hit that amount, 100 percent coverage should kick in. Remember, these costs all depend on what kind of plan you have.
Is Medigap more expensive than Part C?
A Medigap plan is generally a little more expensive than a Part C plan and doesn’t include prescription drugs. But it may be the most stress-free way to ensure that all cancer treatment costs are handled through your coverage.
Does Medicare cover radiation?
Medicare covers radiation treatments, but you’ll be responsible for any out-of-pocket costs after your plan has paid its share. Medigap plans can reduce or eliminate out-of-pocket costs for your treatments. Cancer treatments can get expensive quickly, especially when you need regular chemotherapy or radiation therapy.
How much is radiation therapy for Medicare?
When someone with original Medicare undergoes radiation therapy in an outpatient clinic or doctor’s office, their out-of-pocket costs include a $198 deductible and a 20% coinsurance. Out-of-pocket costs of Medicare Advantage plans are different. A person may wish to check their plan to get an idea of the expenses to expect.
What is a Medigap plan?
Medigap. Medigap is Medicare supplement insurance, which is available for purchase to a person with original Medicare. The plans cover 50–100% of out-of-pocket costs associated with parts A and B, including those for cancer treatment.
How much is Part A coinsurance?
Part A costs include: $1,408 deductible for each benefit period. $0 coinsurance for the first 60 days of a benefit period. $352 per day coinsurance for days 61 to 90 of a benefit period. A benefit period starts the day a person enters a hospital and ends the day after they have been home from the hospital for 60 consecutive days.
What is covered by Part A?
Other possible cancer-related coverage of Part A includes blood, home health, and hospice care. Part B covers radiation therapy in an outpatient clinic, along with the services below: many chemotherapy drugs given to a person through the vein. some chemotherapy drugs that are taken by mouth. outpatient surgeries.
Why do doctors recommend radiation therapy?
Doctors advise radiation therapy for four purposes: to shrink early stage cancer. to lower the risk that cancer will recur. to reduce symptoms caused by advanced cancer.
What are the programs that help pay for people with limited means?
The following programs can help pay the costs for people with limited means: Medicare savings programs help pay some deductibles, copayments, coinsurance, and premiums. Each of the four programs has eligibility requirements that depend on someone’s income and resources.
What do you need to know before buying a Part D insurance?
Before buying a Part D plan, a person may wish to check the policy formulary. Formularies are lists of medications that a plan covers, and they often differ between plan providers. Other cancer-related drugs that Part D may cover include medications for nausea and pain.
How do health insurers ration care?
They will only pay for you to visit the ones they have negotiated the lowest fees with. 3 . Health insurers ration care through co-pays, deductibles, and caps.
What is healthcare rationing?
Healthcare rationing is used by health insurers, the government, and individuals to save money. Some would even argue healthcare rationing supports the greater good. Uppercut Images / Getty Images.
What is the difference between government rationing and rationing?
The difference between the government's rationing and the rationing conducted by health insurers is that there is no profit motive. The government, through Medicare or state Medicaid or other programs, keeps costs lower as much as possible in order to keep taxes lower or to expand care to others, both considered to be the greater good.
Why do insurance companies ration care?
When insurance companies ration care, it's a money-saving measure, in part for the greater good, but also to preserve profits or raise salaries or other reasons that their customers disdain. Some of their rationing does keep premiums from getting even higher, and also allows insurers to stay in business.
How can understanding healthcare rationing help you?
There are several reasons why understanding healthcare rationing will help you. Should you run into a denial of care, you'll know why it's been denied, and will better understand how to go about combating it, should you want to do so.
Why is denial of care considered rationing?
Denial of care is perhaps the most understood form of rationing because it causes outrage and frustration. What most patients don't understand is that this is also the aspect of rationing that is most affected by laws and regulations, too.
What does "rationing" mean in the military?
Elaine Hinzey is a fact checker, writer, researcher, and registered dietitian. Rationing means that you are limited in what you are allowed to purchase. It was used during World War II to ensure the troops had enough supplies while those at home could only buy limited quantities of butter, sugar, or gasoline.
What is Medicare for rehab?
Medicare if a federal health insurance program that help people over the age of 65 afford quality healthcare. Find out about eligibility and how Medicare can help make the cost of rehab more affordable.
How many hours of treatment is required for partial hospitalization?
A physician must certify that individuals in partial hospitalization require that form of treatment, and the person’s plan of care must include at least 20 hours of treatment per week. 5. Services offered in partial hospitalization programs include: 5. Individual and group therapy. Occupational therapy.
What is the Medicare number for substance use disorder?
If you’re battling a SUD or an AUD and qualify for Medicare benefits, please reach out to one of our admissions navigators at. (888) 966-8152.
What is a brief intervention?
Screening, Brief Intervention, and Referral to Treatment (SBIRT) is a screening and intervention technique that can help identify individuals at risk of experiencing alcohol related health issues prior to the need for more comprehensive substance abuse treatment. This type of intervention can be covered by Medicare as a preventive measure when someone in a primary care setting shows signs of substance abuse. 5
What is Part B in Medicare?
Part B helps with payment for outpatient treatment services through a clinic or a hospital outpatient center. Part D can be used to help pay for drugs that are medically necessary to treat substance use disorders.
How old do you have to be to qualify for Medicare?
You may be eligible for Medicare if: 1. You are age 65 or older. You are younger than 65 and have a disability. You are younger than 65 and have end stage renal disease (permanent kidney failure that requires dialysis or a transplant).
Is addiction covered by Medicare?
But there are rules about the providers people can use with Medicare, and some types of addiction treatment are not covered by Medicare at all. It is a good idea to contact the Medicare organization directly to find more detailed information. You are age 65 or older.
Why do countries ration?
While other countries may ration because of national budget constraints and supply-side factors, the United States’ lack of access to comprehensive insurance and affordable care represent a de facto form of rationing that leads people to delay getting care or going without it entirely.
Do Brits pay for hospital care?
In the U.K., Germany, and the Netherlands, patients have no out-of-pocket costs when they visit a primary care doctor, and Brits never pay for hospital care. In Germany, out-of-pocket costs are capped at 2 percent of annual household income and 1 percent for chronically ill people.
What happens if a managed care plan doesn't pay for a drug?
Most managed care health plans restrict coverage to a list of certain drugs. If your physician prescribes a drug that’s not on your health plan’s drug formulary, your health plan won’t pay for it, although there is an appeals process and you and your physician can use if no other medication will work. 3. Step therapy.
What did Sarah Palin say about the Affordable Care Act?
Sarah Palin tapped into that sentiment when she claimed in 2009 that the Affordable Care Act would create “death panels” that would decide who would get care and who would be left to die without care. 7. It would be nice if the world had unlimited resources and everyone could have everything they want.
What is managed care?
Health insurers used several techniques to control costs, creating a whole new genre of health insurance products and healthcare delivery methods known collectively as managed care . The idea was that, by managing the care that was provided, the insurer would also be managing the cost of care.
What is restrictive provider network?
Restrictive provider networks requiring you to use only in-network providers for your health care if you want your health insurance company to pay for your care. This is common in HMOs and EPOs. The waiting list for an organ transplant. Health insurance companies aren’t the source of all healthcare rationing in the United States.
Is rationing healthcare necessary?
In some ways, yes. Rationing care helps us to use our limited resources more wisely, picking and choosing among options and trying to get only the care that’s truly necessary. Ultimately, healthcare rationing is a necessary evil. We’ve been living with it since our ancestors paid the town doctor with chickens.
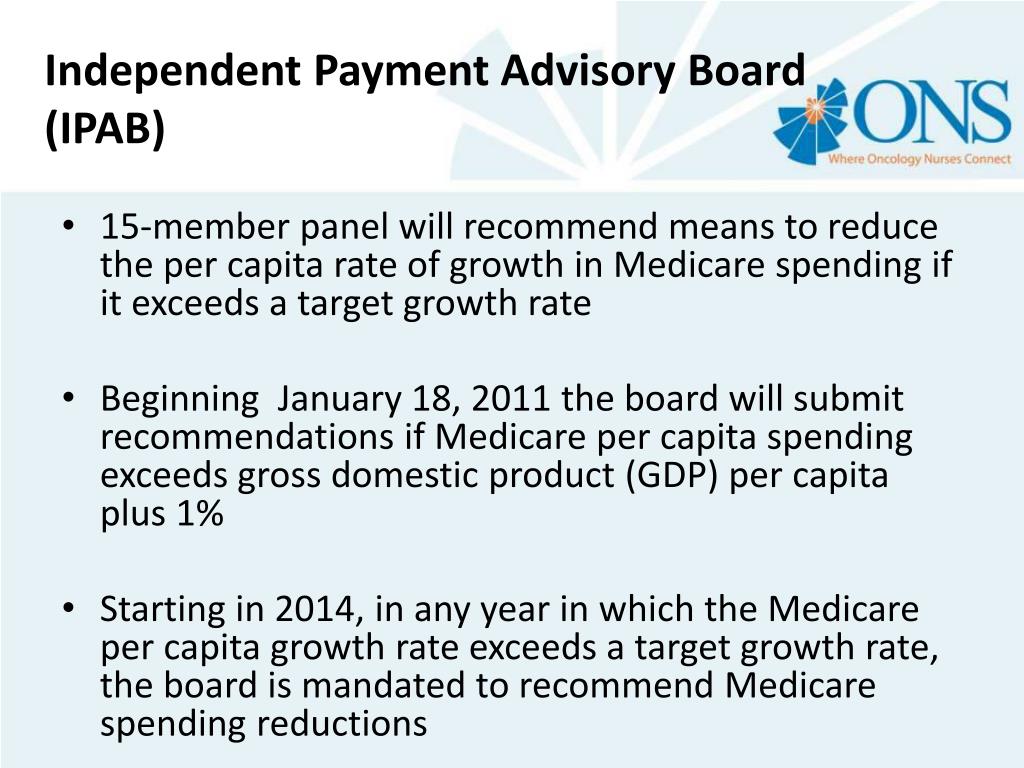
Did the federal government feel the pinch of increasing healthcare costs?
Even the federal government felt the pinch of increasing healthcare costs as it saw Medicare spending increase. Businesses looked for less expensive employee health insurance options. Health insurance companies innovated to fill the need for health insurance that kept healthcare costs in check while delivering quality care.
Should health care be a human right?
Many people feel health care should be the exception to capitalism, it should be a basic human right provided to everyone because people cannot live without health care. However, in the United States many things people cannot live without are rationed economically.
What is a Medigap plan?
Medigap, or Medicare supplemental insurance, is an add-on plan that helps cover some of the costs from your other Medicare plans. If you need treatment for substance use disorder, having a Medigap plan may help cover some of your costs, such as: your Medicare Part A deductible and coinsurance. your Medicare Part B deductible, premium, ...
What does Medicare Part C cover?
Medicare Part C covers anything already included under Medicare parts A and B, plus extras like prescription drug coverage. Medicare Part D covers certain prescription drugs that may be necessary in the treatment of substance use disorder.
What is not covered by Medicare?
What's not covered. Substance use disorder. Takeaway. Substance use disorder — formerly known as substance, drug, or alcohol abuse — affected roughly 20.4 million people in 2019. If you are a Medicare beneficiary, you may be wondering if Medicare covers treatment for substance use disorder. Both original Medicare and Medicare Advantage plans cover ...
How much is Part A in 2021?
For Part A, this is $1,484 per benefit period in 2021. Coinsurance. If your inpatient stay lasts longer than 60 days, you’ll pay $372 each day from days 61 to 90 and $742 per each lifetime reserve day used during the benefit period (up to 60 days over your lifetime).
Does Medicare cover prescription drugs?
Prescription drugs for substance use disorder. Medicare Part D is an add-on to original Medicare that helps cover the cost of prescription drugs. This can be used to cover medications you need during treatment for substance use disorder. Most Medicare Advantage, or Medicare Part C, plans also offer prescription drug coverage.
Does Medicare cover partial hospitalization?
partial hospitalization (intensive outpatient drug rehab) outpatient hospital services. In some instances, Medicare will also cover services related to Screening, Brief Intervention, and Referral to Treatment (SBIRT). These services are intended to help those who may be at risk of developing substance use disorder.
Does Medicare cover substance use disorder?
If you are a Medicare beneficiary, you are covered for many of the treatment options currently available for substance use disorder. Here’s how Medicare covers you for these treatments: Medicare Part A covers inpatient hospital care and inpatient care in a rehabilitation facility or hospital. Medicare Part B covers outpatient mental health ...
What is the benefit period for Medicare?
benefit period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
What is part A in rehabilitation?
Inpatient rehabilitation care. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
Does Medicare cover private duty nursing?
Medicare doesn’t cover: Private duty nursing. A phone or television in your room. Personal items, like toothpaste, socks, or razors (except when a hospital provides them as part of your hospital admission pack). A private room, unless medically necessary.
Does Medicare cover outpatient care?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.