Infants in the early, or aggressive, treatment group received phototherapy if their bilirubin levels reached 5 milligrams per deciliter—a level that previous studies suggested might result in permanent brain damage. Infants in the conservative treatment group received phototherapy when their levels reached 8 milligrams per deciliter.
Full Answer
How to treat and control elevated bilirubin levels in adults?
Treatments for elevated bilirubin not caused by an immature liver could include:
- Antibiotics for infection
- Changing medications if they caused the elevated levels
- Medications, such as corticosteroids, to reduce inflammation in the liver
- Surgery to remove gallstones or gallbladder
- Surgery to remove liver or pancreatic obstructions
What is dangerous level of bilirubin in adults?
What is a dangerous level of bilirubin in adults? A bilirubin level of 5 mg % is considered as dangerous and need to be properly investigated to know the underlying pathology for excess bilirubin production in the body or defective and inefficient bilirubin excretion from the body in the form of further degradation product. Explore further
What medications increase bilirubin?
- Medications
- Inherited or autoimmune liver disease
- Malnutrition
- Rapid weight loss
- Viral hepatitis
How to lower bilirubin levels?
You can help lower your bilirubin levels by:
- Taking deep breaths
- Doing yoga
- Meditating
- Getting a massage
- Listening to music
What is the common treatment for reducing hyperbilirubinemia?
Phototherapy is treatment with a special type of light (not sunlight). It's sometimes used to treat newborn jaundice by making it easier for your baby's liver to break down and remove the bilirubin from your baby's blood.
How long does bilirubin treatment take?
Treatment in the hospital most often lasts 1 to 2 days. Your child needs treatment when their bilirubin level is too high or rising too quickly. To help break down the bilirubin, your child will be placed under bright lights (phototherapy) in a warm, enclosed bed.
What is the danger of hyperbilirubinemia?
What are possible complications of hyperbilirubinemia in a newborn? High levels of bilirubin can travel to your baby's brain. This can cause seizures and brain damage. This is called kernicterus.
What happens if you don't treat hyperbilirubinemia?
This yellow coloring is called jaundice. When severe jaundice goes untreated for too long, it can cause a condition called kernicterus. Kernicterus is a type of brain damage that can result from high levels of bilirubin in a baby's blood. It can cause athetoid cerebral palsy and hearing loss.
How long does it take for bilirubin levels to return to normal?
In most cases, higher bilirubin levels will lead to jaundice between 1 and 3 days after birth. Bilirubin levels can peak as high as 18 mg/dL in the fourth or fifth day, and the jaundice typically clears up within 2 weeks as the liver matures.
How quickly does bilirubin drop with phototherapy?
The overall rate of decrease in the bilirubin concentration for the duration of exposure to phototherapy was as follows: group 1, 0.8%±0.3% per hour; group 2, 0.6%±0.3% per hour; and group 3, 0.8%±0.3% per hour.
Can hyperbilirubinemia be cured?
Symptoms will usually resolve without treatment in mild cases. However, infants with extremely high bilirubin levels will require treatment with either a blood transfusion or phototherapy. In these cases, jaundice treatment in newborns is vital to help prevent kernicterus.
Can hyperbilirubinemia cause brain damage?
In newborn babies with very high levels of bilirubin in the blood (hyperbilirubinaemia), the bilirubin can cross the thin layer of tissue that separates the brain and blood (the blood-brain barrier). The bilirubin can damage the brain and spinal cord, which can be life-threatening.
How long does hyperbilirubinemia last?
Jaundice usually appears about 2 days after birth and disappears by the time the baby is 2 weeks old. In premature babies, who are more prone to jaundice, it can take 5 to 7 days to appear and usually lasts about 3 weeks.
At what level does bilirubin cause brain damage?
Kernicterus, or bilirubin encephalopathy, is bilirubin-induced neurological damage, which is most commonly seen in infants. It occurs when the unconjugated bilirubin (indirect bilirubin) levels cross 25 mg/dL in the blood from any event leading to decreased elimination and increased production of bilirubin.
How high is bilirubin before death?
An elevation greater than 20 mg/dL suggests severe liver disease. In patients with hepatitis-induced acute liver failure, a serum total bilirubin level > 17.5 mg/dL (300 mmol/L) is a criterion for predicting death and the need for liver transplantation.
Is jaundice life threatening in adults?
Is it fatal? The prognosis for individuals with jaundice depends on the underlying cause of the condition. There are certain conditions that carry an excellent prognosis with individuals making a full recovery. However, more serious causes of jaundice can sometimes be fatal despite medical or surgical intervention.
Abstract
The indications for the treatment of hyperbilirubinemia and the methods used for treatment vary according to the individual circumstances.
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
What is hyperbilirubinemia?
Introduction. Hyperbilirubinemia is a condition defined as elevated serum or plasma bilirubin levels above the reference range of the laboratory, and it is due to disorders of bilirubin metabolism. Depending on the form of bilirubin present in serum, hyperbilirubinemia can be further classified as unconjugated (indirect) or conjugated (direct).
Why do newborns have unconjugated hyperbilirubinemia?
Most of the newborn develops unconjugated hyperbilirubinemia (neonatal jaundice) because of hepatic immaturity and low activity of UGT1A1 during days 2 to 5. Breast milk feeding increases bilirubin levels in infants that result in maternal milk jaundice.
What is the normal bilirubin level for CNS2?
Individuals with Crigler-Najjar type II (CNS2) have less than 10% of the normal UGT1A1 activity, resulting in bilirubin levels of 5 to 25 mg/dL. Kernicterus is rare in Crigler-Najjar type II, but patients with increased bilirubin levels (greater than 15 mg/dL) have high chances of its occurrence.
How long does phototherapy help with crigler-najjar syndrome?
To maintain the levels of unconjugated hyperbilirubinemia below the neurotoxic threshold patients with Crigler-Najjar syndrome type I generally need phototherapy for 10 to 12 hours a day. Phototherapy helps in converting bilirubin to more water-soluble bilirubin isoforms that can get excreted in the urine.
What is the effect of decreased bilirubin delivery to the liver?
The impaired hepatic uptake of bilirubin can be the result of decreased bilirubin delivery to the liver and inefficient uptake of bilirubin by hepatocytes, usually resulting from reduced hepatic blood flow (congestive heart failure and portosystemic shunts) and drugs/contrast administration.
What is Lucy Driscoll syndrome?
Lucy-Driscoll syndrome, also known as Maternal serum jaundice, a form of transient familial neonatal unconjugated hyperbilirubinemia, is a rare metabolic disorder caused by a UGT1A1 inhibitor usually present in the maternal serum.
What enzyme converts heme to bilirubin?
The conversion of heme to bilirubin is a two-step reaction, in the first step the microsomal heme oxygenase enzyme of the reticuloendothelial system, converts heme to biliverdin, which in turn is reduced to unconjugated bilirubin (UCB) by a second enzyme biliverdin reductase.[7] . The UCB is lipophilic.
How to diagnose hyperbilirubinemia?
Diagnostic procedures for hyperbilirubinemia may include: 1 Direct and indirect bilirubin levels. A blood test can determine if the bilirubin is bound with other substances by the liver so that it can be excreted (direct), or is circulating in the blood circulation (indirect). 2 Red blood cell count may be used to determine if the baby has too many or too few red blood cells. 3 Reticulocyte count determines the number of young red blood cells, which is an indication of red blood cell production. 4 Blood type and testing for ABO or Rh incompatibility (Coomb's test)
What is the procedure to test for hyperbilirubinemia?
Diagnostic procedures for hyperbilirubinemia may include: Direct and indirect bilirubin levels. A blood test can determine if the bilirubin is bound with other substances by the liver so that it can be excreted (direct), or is circulating in the blood circulation (indirect).
What is physiologic jaundice?
Physiologic jaundice occurs as a "normal" response to the baby's limited ability to excrete bilirubin in the first days of life due to the immaturity of the liver. This will usually resolve by the first week of life. Breastfeeding failure jaundice. During the first few days of breastfeeding when the maternal breast milk supply ...
How to tell if a baby has high bilirubin?
Elevated bilirubin is evident by yellow discoloration of the baby's eyes, mucosa and skin, usually starting from the head and moving downward. Prior to discharge in the hospital, most babies will have their bilirubin level checked, either by a skin (transcutaneous) probe or a blood test. Other symptoms of jaundice may include poor feeding ...
How long does it take for breast milk to cause jaundice?
About 2 percent of breastfed babies develop jaundice after the first week. It peaks about two weeks of age and can persist up to three to twelve weeks. Breast milk jaundice is thought to be caused by a substance in the breast milk that increases the reabsorption of bilirubin through the intestinal tract.
What is the process of bilirubin?
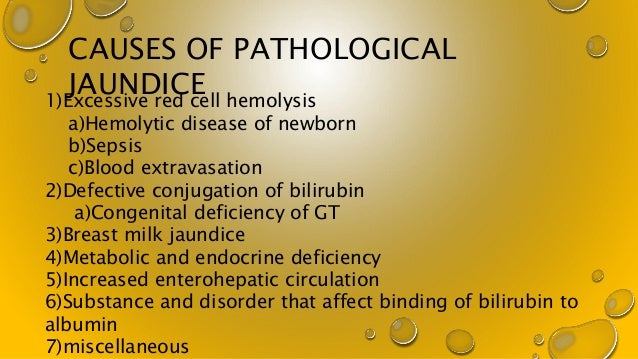
Bilirubin is a natural byproduct produced when red blood cells breakdown. The adult liver converts unconjugated bilirubin into a conjugated form, that be excreted. During pregnancy, the placenta excretes bilirubin but when the baby is born, the baby's immature liver must assume that role. There are several causes of hyperbilirubinemia and jaundice, ...
Why does jaundice occur?
Jaundice may occur if there is an increase of red blood cell breakdown (hemolysis) such as that seen when there is a mismatch of maternal and fetal blood type , resulting in ABO incompatibility or hemolytic disease of the newborn (Rh disease). Increased hemolysis can also occur if the baby is bruised or develops a hematoma during delivery.
Why is bilirubin action limit important?
Use of bilirubin action limits. Due to the extensive use of action limits, accuracy and precision of the measurement of bilirubin are important. The overestimation of bilirubin could potentially lead to unnecessary therapy.
What happens when bilirubin absorbs blue light?
This type of therapy is relatively harmless. The major disadvantage is the disruption of the contact between the mother and the child and a mild dehydration.
Why do neonates have jaundice?
HYPERBILIRUBINEMIA IN THE NEONATE. 60 % of all neonates develop jaundice during their first week of life due to factors such as: Natural rate of bilirubin production being greater per body mass compared with adults. Hyperbilirubinemia may in severe cases lead to kernicterus.
How many neonates develop jaundice?
60 % of all neonates develop jaundice during their first week of life and thereby run a risk of getting hyperbilirubinemia. Although different approaches for establishing treatment criteria have been suggested, treatment of neonatal hyperbilirubinemia is usually still based on the measurement of total bilirubin concentration.
What is the major part of bilirubin?
The major part (80 %) of bilirubin is produced by the degradation of the heme group of hemoglobin. The rest is derived from erythrocyte precursors or from the degradation of other heme-containing proteins.
Is bilirubin soluble in water?
Unconjugated bilirubin – also called indirect bilirubin. It is poorly soluble in water and a high concentration of this is toxic due to its solubility in fatty tissue. Unconjugated bilirubin bound to albumin. It is water-soluble and non-toxic. Conjugated bilirubin – also called direct bilirubin.
Does acid-base status affect bilirubin?
There is also some evidence that acid-base status [1,27,28] and hypoxia [29] affect the toxicity of bilirubin. It is not enough to strive for getting an accurate and precise bilirubin determination that can justify the use of specific action limits together with an evaluation of the general status.
What causes conjugated hyperbilirubinemia?
In most patients, the cause of conjugated hyperbilirubinemia is apparent, such as those with viral hepatitis or sepsis. When this is not the case or when multiple causes are possible, consultation with a gastroenterologist or a hepatologist may be helpful.
Can hepatotoxic drugs cause liver failure?
For this reason, it is best to stop all potentially hepatotoxic drugs until the cause of the conjugated hyperbilirubinemia can be determined.