See more
How is ACE angioedema treated?
Corticosteroids, antihistamines, and epinephrine still are used for the initial treatment of ACEI angioedema; however, no specific guidelines have been published in the United States.
How does ACE inhibitor cause angioedema?
ACE inhibitor-induced angioedema is due to the inhibition of bradykinin degradation resulting in elevated plasma bradykinin. As most people on ACEi are able to normalise the bradykinin level by other pathways, a genetic susceptibility is assumed.
What should be done if a patient experiences angioedema from use of an ACEi?
If angioedema develops in a patient on an ACEi, the ACEi should be discontinued and a different antihypertensive class used. HAE is thought to be autosomal dominant with abnormal C1-INH amounts and/or function.
How is bradykinin induced angioedema treated?
Initial evaluation should focus on airway management and treatment with epinephrine, antihistamine and systemic steroids according to anaphylactic protocols, except for known HAE patients and individuals with a history of drug-induced angioedema.
Why does FFP help angioedema?
Therefore, the rationale for using FFP in ACEI-associated angioedema is that it contains kininase II, which is similar to angiotensin-converting enzyme and catalyzes the degradation of excessive bradykinin, thus rendering it ineffective.
Why ACE inhibitors cause dry cough and angioedema?
The means by which ACE inhibitors affect the respiratory system is thought to be through an increase of substance P, which is released from the vagal and glossopharyngeal sensory nerves in the pharynx and upper airways, and is naturally degraded by ACE [7,47]. In this case, this will increase the cough reflex.
Can an ARB be given to patients who have had angioedema on an ACE inhibitor?
current evidence suggests no ab- solute contraindication to angiotensin receptor blockers (ARBs) in patients who have had angioedema attributable to an angioten- sin-converting enzyme (ACE) inhibitor.
Why does ARB cause angioedema?
Angioedema associated with angiotensin converting enzyme inhibitors (ACEIs) is due to the accumulation of bradykinin and its metabolites. Angiotensin receptor blockers (ARBs) produce anti-hypertensive effects by blocking the angiotensin II AT1 receptor action; hence bradykinin-related side effects are not expected.
Do ARBs increase bradykinin?
An increase in bradykinin levels results in continued prostaglandin E2 synthesis, vasodilation, increased vascular permeability, and increased interstitial fluid. In contrast, the angiotensin II receptor blockers (ARBs) do not increase bradykinin levels.
What medications block bradykinin?
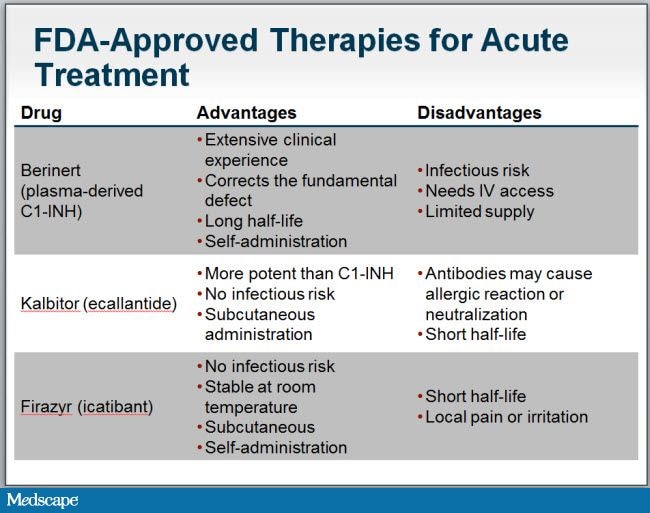
Bradykinin receptor antagonists such as icatibant inhibit bradykinin from binding the B2 receptor and thereby treat the clinical symptoms of an acute attack. Recommended dose of icatibant is 30 mg SC in the abdominal area. It is available as a single-use, prefilled syringe, which delivers a dose of 30 mg (10 mg/mL).
Do antihistamines reduce bradykinin?
Antihistamines, namely Dimedrol (diphenhydramine), Diprazin (Pipolphen), Tavegyl, and Suprastin, reduced the spasmogenic effects of bradykinin and the increased permeability of the microvessels caused by this polypeptide, in isolated segments of guinea pig ileum and also in rats and guinea pigs.
What is the treatment for angioedema?
Treatment modalities include antihistamines, steroids, and epinephrine, as well as endotracheal intubation in cases of airway compromise. Patients with a history of ACE-I-induced angioedema should not be re-challenged with this class of agents, as there is a relatively high risk of recurrence.
Is ACE I used for angioedema?
ACE-I are frequently used therapeutic agents that are associated with angioedema. Their use should be avoided in high-risk individuals and early diagnosis, tracheal intubation in cases of airway compromise, and absolute avoidance of re-challenge are important. ACE-I are frequently used therapeutic agents that are associated with angioedema.
What percentage of angioedema is caused by ACE inhibitors?
● The overall incidence of angioedema in patients receiving angiotensin-converting enzyme (ACE) inhibitors is between 0.1 and 0.7 percent. ACE inhibitors are the leading cause of drug-induced angioedema, accounting for up to 40 percent of emergency visits for angioedema. (See 'Epidemiology' above.)
What is the clinical feature of ACE inhibitor-induced angioedema?
The clinical features of ACE inhibitor-induced angioedema are related to elevated levels of bradykinin, an inflammatory vasoactive peptide, which leads to vasodilation of blood vessels. The pathways involved in bradykinin generation are described briefly here.
How long does it take for angioedema to develop after ACE?
In more than one-half of the case reports of visceral angioedema, symptoms began within 72 hours of starting ACE inhibitor therapy, although in other reports, angioedema developed after weeks or years of therapy [ 28,29,35 ]. The jejunum is most often involved, followed by the ileum and duodenum.
What is the leading cause of drug-induced angioedema in the United States?
Although the risk to an individual is relatively low, the large number of people taking these medications means that ACE inhibitors are the leading cause of drug-induced angioedema in the United States, accounting for 20 to 40 percent of all emergency department visits for angioedema each year [ 14-16 ].
What parts of the body are affected by ACE inhibitors?
The reason that these particular parts of the body are more often affected is not known. Face, mouth, and upper airway — The edema that occurs from ACE inhibitors usually affects the lips, tongue, and face ( picture 1) [ 19 ]. Angioedema of the pharynx, larynx, and subglottic area have also been reported.
What is the most affected area of the body with ACE inhibitor?
Affected areas — ACE inhibitor-induced angioedema most commonly affects the lips, tongue, face, and upper airway. The intestine can also be involved, presenting as acute abdominal pain with diarrhea or other gastrointestinal symptoms, but this presentation may be less well recognized.
What is ACE inhibitor used for?
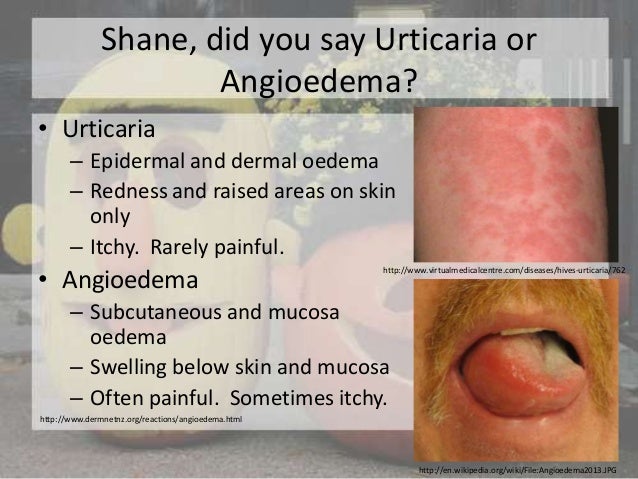
ACE inhibitors are routinely used in patients with hypertension, myocardial infarction, heart failure, diabetes, and chronic kidney disease. CLINICAL FEATURES. —. Angioedema is an asymmetric, nonpitting swelling of the subcutaneous or submucosal tissues that most commonly affects nondependent areas.
What is the risk of angioedema in ACE?
Factors recognised to increase the risk of developing ACE inhibitor-induced angioedema include: African descent. Age over 65 years. Female.
When does angioedema start?
Episodes of angioedema usually begin in the first month after starting the ACEi, but onset can be delayed by months or years.
What is the safest replacement for ACEI?
The safest replacement for the ACEi would be an angiotensin receptor blocker (ARB). Treatments for hereditary angioedema have been tried — fresh frozen plasma, plasma-derived C1 inhibitor concentrate, tranexamic acid, ecallantide, and/or icatibant. However, strong evidence to support their use in ACE inhibitor-induced angioedema is lacking.
What is angioedema in the mouth?
Angioedema is an acute, transient, localised deep swelling of skin or mucous membranes, typically affecting loose areas of tissue in non- dependent areas, and not usually associated with itch or urticaria. ACE inhibitor-induced angioedema can involve: Oral mucosa and upper airways including swelling of the lips, tongue, and floor of mouth.
What are the symptoms of angioedema in the upper airways?
Oral mucosa and upper airways including swelling of the lips, tongue, and floor of mouth. Symptoms may include dyspnoea, dysphagia, stridor, and hoarseness. Swelling around the eyes is uncommon in ACE inhibitor-induced angioedema.
Does ACE cause angioedema?
It is important to note ACE inhibitor-induced angioedema does not involve histamine.
Can ACE inhibitors cause angioedema?
ACE inhibitor-induced angioedema is a rare but potentially fatal adverse effect of the class of medications that inhibit angiotensin converting enzyme (ACEi). It typically presents in the first weeks after starting the ACEi as swelling of the face, lips, or tongue in the absence of itch or urticaria.
How long does it take for angioedema to resolve?
Angioedema can develop over minutes to hours, and typically resolves in 1 to 2 days. Although usually self-limiting, it can be life-threatening—especially if it goes unrecognized and untreated. ACE inhibitor-related angioedema usually arises shortly after drug therapy begins, but in some cases it’s delayed for months or even years.
Why are ACE inhibitors ineffective?
However, these drugs may be ineffective because inflammatory mediators other than histamine appear to be the basis for angioedema caused by ACE inhibitors. I.V. corticosteroids and subcutaneous epinephrine are reserved for more severe episodes.
What is the ACE inhibitor?
Chances are, you’ve administered angiotensin-converting enzyme (ACE) inhibitors, such as captopril, enalapril, or lisinopril, to many patients. Worldwide, more than 40 million people take these drugs—most of them to treat heart failure or hypertension, especially after myocardial infarction. These drugs also are given for coronary artery disease, ...
Can ACE inhibitors cause angioedema?
For patients who need ACE inhibitors despite a high risk for angioedema —for instance, those who’ve had previous idiopathic angioedema—provide an epinephrine kit, as ordered, and give instructions on how to use it.
Can pruritus cause angioedema?
However, pruritus or urticaria usually accompany angioedema from these causes. The physician also must rule out idiopathic angioedema and C1 esterase inhibitor deficiency—a hereditary or acquired condition that disrupts the pro-inflammatory response, causing recurrent angioedema.
Can you stop an ACE inhibitor?
In most cases, stopping the ACE inhibitor is the only treatment needed. However, be sure to evaluate the patient for airway compromise, and be prepared to intervene appropriately. A patient with significant airway compromise that threatens ventilation should be hospitalized for careful observation, with an intubation tray kept near the bedside. Be aware that nasotracheal intubation is recommended, as nonpitting edema can make oral intubation difficult or even impossible.
What is the first priority for ACE inhibitor induced angioedema?
When you encounter a patient with ACE inhibitor induced angioedema that involves the upper airway, the first and only priority is to protect the patient’s airway.
How long does angioedema last after stopping ACE?
Symptoms can persist for up to 6 weeks after stopping ACE inhibitors, and this complicates the assessment of cross-reactivity with other medications such as angiotensin receptor blockers (ARB).
How long does it take for an ACE inhibitor to cause swelling?
Swelling usually develops over minutes to hours, peaks, and then resolves over 24 to 72 hours. There are no definitive tests to confirm ACE inhibitor induced angioedema.
Is ecallantide a hereditary drug?
Ecallantide. Ecallantide is also approved for hereditary angioedema. It differs from icatibant in that it inhibits the unregulated production of bradykinin by inhibiting kallikrein. It appears that ecallantide is not effective for the treatment of ACE inhibitor induced angioedema.
Can ACE inhibitors cause angioedema?
Because of the high frequency of ACE inhibitor use, many patients will go on to develop ACE inhibitor induced angioedema.
Can you switch to ARB for ACE inhibitor?
It is generally recommended that patients with ACE inhibitor induced angioedema should only switch to an ARB if they also have a compelling indication such as heart failure or chronic kidney disease.
