No. Hepatitis
Hepatitis
Inflammatory condition of the liver.
How is hepatitis C virus (HCV) (HIV) infection treated in HIV infection?
Antiretroviral treatment for HIV may slow the progression of HCV-related liver disease and reduce the risk of liver-related morbidity. For all persons with HIV-HCV coinfection, antiretroviral therapy should be initiated to treat HIV, regardless of the CD4 cell count and fibrosis stage.
Are there any new treatments for hepatitis C?
However, new treatments for hepatitis C have been approved in recent years. These direct-acting antiviral treatments are much better than the previously available treatment because they have few side effects and do not need to be injected.
When should people with HIV and hepatitis C co-infection start antiretroviral treatment?
Like everyone else living with HIV, people with HIV and hepatitis C co-infection are advised to start antiretroviral treatment soon after being diagnosed with HIV. People with co-infection may particularly benefit from early treatment because having well-controlled HIV and restored immune function reduces the risk of liver disease progression.
What are the treatment options for HIV-HBV and HCV?
If you continue injecting drugs, always use new, sterile needles or syringes, and never reuse or share needles or syringes, water, or other drug preparation equipment. HIV-HBV and HIV-HCV coinfections can be effectively treated in most people.

Can you treat Hep C and HIV at the same time?
People on antiretroviral treatment for HIV can be successfully treated for hepatitis C at the same time. Given the number and variety of HIV and hepatitis C medications now available, most people with co-infection can put together well-tolerated regimens for treating both viruses.
How long live with HIV and Hep C?
Among patients living with HIV, HCV coinfection is associated with a median life expectancy decrease of 17.3 years and low probability of surviving until the age of 65 years. In the era of directly acting anti-HCV drugs, treatment scale-up and immediacy of treatment are advisable in this cohort.
Can Hep C affect HIV test?
It is not possible to know if you have HIV or hepatitis C unless you have a blood test. A blood test will check whether you have hepatitis C and/or HIV. need a blood test that specifically looks for the hepatitis C virus.
Can you have HIV and hepatitis at the same time?
According to the Centers for Disease Control and Prevention (CDC), approximately 10% of people with HIV in the United States also have HBV. Infection with both HIV and HBV is called HIV/HBV coinfection.
How long does hep C take to damage liver?
On average it takes about twenty years for significant liver scarring to develop. The symptoms experienced and the damage done to the liver vary dramatically from person to person. Some people will have few, if any, symptoms for many years.
What is the life expectancy of someone with hep C?
The prognosis of chronic HCV is typically very good, and as treatment continues to improve, it will only get better. Most people with chronic HCV can live a normal life, providing that doctors are able to diagnose it before any liver damage or other complications occur.
How long can you live without Hep C treatment?
Like the human papillomavirus (HPV), early acute hepatitis C can clear on its own without treatment; this happens about 25% of the time. However, it's more likely that the virus will remain in your body longer than six months, at which point it's considered to be chronic hepatitis C infection.
What is the drug for hepatitis C?
Newer drugs for the treatment of hepatitis C, such as the combinations of glecaprevir/pibrentasvir ( Maviret) and sofosbuvir/velpatasvir/voxilaprevir ( Vosevi) may become available in some parts of the UK in 2018, subject to funding arrangements.
How long does it take to cure hepatitis C?
On the other hand, people who are more difficult to treat may need to lengthen treatment to 16 or 24 weeks.
What is the most common type of hepatitis C?
Genotype 4 is the most common type of hepatitis C in the Middle East and North Africa, but it has also been seen in hepatitis C outbreaks in the UK and Europe. Genotype 4 generally responds to the same DAAs as genotype 1. Genotype 5 and 6 are less common and less well studied.
How many genotypes of hepatitis C are there?
This determines which DAAs will work and predicts treatment response. Some DAAs are 'pangenotypic' or active against all genotypes. There are at least six major hepatitis C genotypes. Genotype 1 is the most common type in the UK, Europe and the US.
What are the standards for HIV treatment in the UK?
In the UK, standards for HIV treatment and care are set and monitored by the British HIV Association (BHIVA), the professional association for HIV doctors and other healthcare professionals. The most recent guidelines on HIV and hepatitis co-infection were produced in 2017 (see www.bhiva.org/hepatitis-guidelines.aspx ). Experts now agree that treatment recommendations for people with HIV and hepatitis C should be the same as for everyone else with hepatitis C, so your treatment will follow national guidelines for hepatitis C treatment.
Why do people with HIV need early treatment?
People with co-infection may particularly benefit from early treatment because having well-controlled HIV and restored immune function reduces the risk of liver disease progression. Current guidelines recommend that everyone with HIV and HCV co-infection should start hepatitis C treatment with DAAs.
What is a direct acting antiviral?
Direct-acting antivirals (DAAs) target different steps of hepatitis C reproduction. These include hepatitis C protease inhibitors, polymerase inhibitors and NS5A inhibitors. Recommended regimens include at least two drugs that work in different ways. Using a single medication alone can lead to drug resistance.
How to prevent hepatitis C?
Ways to prevent hepatitis C include: not sharing personal hygiene items, such as toothbrushes and shaving razors. only using qualified and reputable practitioners for tattoos and piercings.
How long does it take to get rid of hepatitis C?
This combination of medications prevents HCV from replicating until the virus is no longer present in the body. Treatment usually takes 6 to 24 weeks but can take longer.
What is coinfection in HIV?
A coinfection is when someone has two or more infections at the same time. People living with HIV are at risk of developing coinfections such as hepatitis C because HIV weakens the immune system, which leaves the body more vulnerable to other infections and illnesses. HIV and HCV are also transmitted in similar ways, ...
How many people in the US have hepatitis C?
In the United States, over a third of people living with HIV also have hepatitis C. Coinfection of HCV and HIV is higher among those who use injected drugs. According to the Centers for Disease Control and Prevention (CDC), HCV coinfection occurs in between 62 and 80 percent. of people with HIV who use injected drugs.
How long does it take to get a HCV treatment?
Treatment usually takes 6 to 24 weeks but can take longer. However, people who have both HIV and HCV need individualized treatments because the medications used to treat HCV infections can interact with HIV treatments. A doctor will recommend a treatment plan based on the individual’s: hepatitis C genotype.
How long does it take for hepatitis C to develop?
Hepatitis C can occur in two forms: Acute. This form of the disease is a short-term infection that usually develops within six months after contracting the virus. In most people, acute hepatitis C usually progresses to the chronic form.
Can HIV be contracted without HIV?
People who have HIV are at higher risk of getting hepatitis C than those without HIV. A person can contract hepatitis C through direct contact with blood that contains HCV. Risk factors for hepatitis C include sharing needles or personal hygiene items, such as razors and toothbrushes.
How long does it take to cure hepatitis C?
In the past, the standard chronic hepatitis C treatment for people co-infected with HIV consisted of weekly injections of a medication called pegylated interferon and a daily dose of the drug ribavirin for 48 weeks. This regimen cured chronic hepatitis C only 20 percent of the time in people with HCV-HIV co-infection. What’s more, the treatment was associated with many side effects, from vomiting, diarrhea, muscle aches and headaches in the short term to depression, anemia, insomnia, weight loss, hair loss, and a drop in the number of infection-fighting white blood cells in the long term.#N#As a result, many physicians and their HCV-HIV co-infected patients did not try to treat chronic hepatitis C at all. Scientists have been working to fill the unmet need for a highly effective, safe and tolerable chronic hepatitis C treatment regimen for people with HCV-HIV co-infection.
Can hepatitis C be treated with HIV?
Hepatitis C can be a chronic condition that leads to liver failure, and treatments often haven’t worked for patients who are also co-infected with HIV. Thanks to research led by the National Institute of Allergy and Infectious Diseases and Gilead Sciences, new therapies are now available that can cure even complicated cases of hepatitis C without serious side effects. Read on to learn how these discoveries were made and what they mean for patients around the world.
Is Sovaldi safe for chronic hepatitis C?
Gilead Sciences, Inc. of Foster City, Calif., makes sofosbuvir, which is now FDA-approved and marketed as Sovaldi .#N#Gilead Sciences launched a clinical trial in 2012 to test the safety and efficacy of a daily regimen of sofosbuvir and ribavirin for treating chronic hepatitis C in people with HIV-HCV co-infection. The 223 participants were taking anti-HIV therapy and had not previously received treatment for hepatitis C. Investigators found that the regimen cured chronic hepatitis C 75 percent of the time in people who were treated for 24 weeks, but led to a cure less often in people who were treated for 12 weeks. Also, the regimen was associated with side effects related to ribavirin, including anemia, fatigue, insomnia, nausea, and headache.
Is ledipasvir safe for cirrhosis?
For safety reasons, the ERADICATE study purposely excluded people with cirrhosis and prior hepatitis C treatment experience. The effectiveness of the ledipasvir/sofosbuvir treatment regimen in such individuals remains an important concern because they represent a significant proportion of the HIV-HCV co-infected people who need treatment. A more recent study conducted by Gilead Sciences addressed this tougher-to-treat population, prescribing ledipasvir/sofosbuvir once daily for 12 weeks to 335 people with HCV-HIV co-infection, some of whom had cirrhosis or past hepatitis C treatment experience, and all of whom were on anti-HIV therapy. Investigators found a chronic hepatitis C cure rate of 96 percent with no serious side effects, boding well for the future treatment of many people with HCV-HIV co-infection.
What is the treatment for HIV and HCV?
These new drugs are often referred to as direct-acting antivirals, or DAAs.
Can you get HCV with DAAs?
Various guidelines around the world now recommend that people who are vulnerable to getting HCV (such as people who inject drugs) be offered an HCV test; that everyone living with HCV be treated – preferably with DAAs – regardless of the liver damage they have suffered ; and that people living with both HIV and HCV be treated for their HCV with the same drugs taken by people who are only living with HCV.
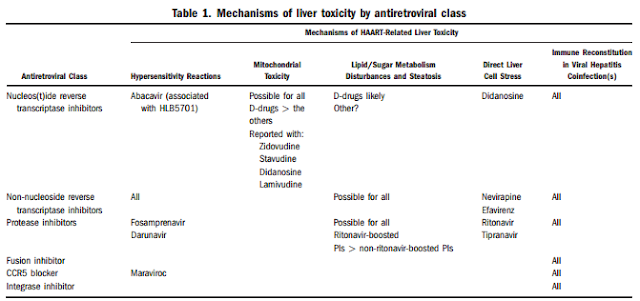
Why do you need to monitor after antiretroviral therapy?
Because of the increased risk of hepatoxicity after initiating antiretroviral therapy in persons with HCV confection, the Adult and Adolescent ARV Guidelines recommend the following monitoring after initiating antiretroviral therapy in persons with HCV-HIV coinfection. [ 33]
What is the AASLD-IDSA HCV guidance?
The AASLD-IDSA HCV Guidance addresses treatment of persons with HCV and HIV coinfection in detail. [ 13] The AASLD-IDSA HCV Guidance recommends using the same general approach for treating HCV in persons with HCV-HIV coinfection as with HCV monoinfection, but notes the importance of recognizing and managing potential drug interactions between HCV medications and HIV antiretroviral medications. [ 13] In most instances, the AASLD-IDSA HCV Guidance recommends using the same HCV treatment regimens and duration for persons with HCV-HIV coinfection as for those with HCV monoinfection, with several exceptions, as outlined below, that require a longer treatment duration for persons with HCV-HIV coinfection than those with HCV monoinfection due to insufficient data on the efficacy of these 8-week regimens among individuals with coinfection. [ 13]
What is glecaprevir pibrentasvir?
Glecaprevir-Pibrentasvir: Glecaprevir is a substrate of OATP1B1/3, p-glycoprotein (P-gp) and breast cancer resistance protein (BCRP), as well as an inhibitor of these transporters. The levels of glecaprevir are increased when used with the HIV protease inhibitors atazanavir, lopinavir, or ritonavir. [ 38] .
Does HIV accelerate hepatic fibrosis?
In persons with chronic HCV, coinfection with HIV accelerates the progression of hepatic fibrosis. Therefore, treatment of both HIV and HCV should have high priority in persons with HIV-HCV coinfection.
Is glecaprevir a contraindication?
Glecaprevir-pibrentasvir is contraindicated for use with atazanavir (with or without ritonavir or cobicistat). In addition, glecaprevir-pibrentasvir is not recommended for coadministration with darunavir, lopinavir, tipranavir, ritonavir, efavirenz, etravirine, or nevirapine.
Can you use ledipasvir with cobicistat?
Because of this concern and lack of data, the use of ledipasvir with the combination of tenofovir DF and cobicistat- or ritonavir-boosted HIV protease inhibitors should, if possible, be avoided. For similar reasons, ledipasvir-sofosbuvir should not be used with cobicistat, elvitegravir, or tipranavir.
How old do you have to be to get tested for hepatitis C?
CDC now recommends one-time hepatitis C testing of all adults (≥18 years of age), including those with HIV. CDC continues to recommend people with risk factors, like people who inject drugs, be tested regularly. The American Association for the Study of Liver Disease (AASLD) and the Infectious Diseases Society of America (IDSA) ...
How common is HCV?
As HCV is a bloodborne virus transmitted through direct contact with the blood of an infected person, coinfection with HIV and HCV is common (62%–80%) among injection-drug users who have HIV [ 8-10 ].
How many people tested positive for HIV in 2009?
In 2009, approximately 21% of adults with HIV who were tested for past or present hepatitis C virus (HCV) infection tested positive, although coinfection prevalence varies substantially according to risk group (e.g., men who have sex with men [MSM], high-risk heterosexuals, and people who inject drugs) [ 7-9 ].
Does the CDC recommend HIV testing?
CDC recommends that people with HIV be tested for hepatitis B. CDC now also recommends one-time hepatitis C testing of all adults (18 years and older), including those with HIV. CDC continues to recommend people with risk factors, like people who inject drugs, be tested regularly.
Do you need IG for HIV?
Therefore, they might need to receive immune globulin (IG) after a high-risk exposure (e. g., a sexual or household contact).
Is HIV a bloodborne virus?
Hepatitis B virus ( HBV) and HIV are bloodborne viruses transmitted primarily through sexual contact and inject ion-drug use. Because of these shared modes of transmission, a high proportion of adults at risk for HIV infection are also at risk for HBV infection. People with HIV who become infected with HBV are at increased risk for liver-related ...
Is HCV a chronic disease?
HCV is one of the primary causes of chronic liver disease in the Unit ed States, and HCV-related liver injury progresses more rapidly among people coinfected with HIV [ 11-15 ]. HCV infection may also affect the management of HIV infection [ 6, 15, 16 ]. CDC now recommends one-time hepatitis C testing of all adults (≥18 years of age), ...
How to prevent hepatitis C infection?
The best way to prevent hepatitis C infection is to never inject drugs or to stop injecting drugs by getting into and staying in drug treatment. If you continue injecting drugs, always use new, sterile needles or syringes, and never reuse or share needles or syringes, water, or other drug preparation equipment.
What is the cause of hepatitis B?
Hepatitis B and hepatitis C are liver infections caused by a virus. Because these infections can be spread in the same ways as HIV, people with HIV in the United States are often also affected by chronic viral hepatitis. Viral hepatitis progresses faster and causes more liver-related health problems among people with HIV than ...
Does hepatitis cause liver disease?
Viral hepatitis progresses faster and causes more liver-related health problems among people with HIV than among those who do not have HIV. Liver disease, much of which is related to HBV or HCV, is a major cause of non-AIDS-related deaths among people with HIV.
Is hepatitis B or C?
Given the risks of hepatitis B or hepatitis C coinfection to the health of people living with HIV, it is important to understand these risks, take steps to prevent infection, know your status, and, if necessary, get medical care from someone who is experienced in treating people who are coinfected with HIV and HBV, or HIV and HCV.
Can HIV be treated?
HIV-HBV and HIV-HCV coinfections can be effectively treated in most people. But medical treatment can be complex, and people with coinfection should look for health care providers with expertise in the management of both HIV infection and viral hepatitis.
Can hepatitis C be left untreated?
Left untreated, it can cause several liver damage, liver cancer, or death. However, new treatments for hepatitis C have been approved in recent years. These direct-acting antiviral treatments are much better than the previously available treatment because they have few side effects and do not need to be injected.
Is hepatitis C tested for HIV?
Is Hepatitis Testing Recommended for People with HIV? Yes. Everyone living with HIV should be tested for HB V and HCV when they are first diagnosed with HIV and begin treatment. People living with HIV who have ongoing risk factors for getting hepatitis B or hepatitis C should be tested annually.