Example letter appealing denial of experimental treatment (Word, 34.00 KB) Out of network Try to show your plan didn’t have access to a provider with the needed specialty in-network, or there was an unreasonably long wait time for an in-network provider. Example of letter seeking payment to an out of network provider (Word, 30.50 KB)
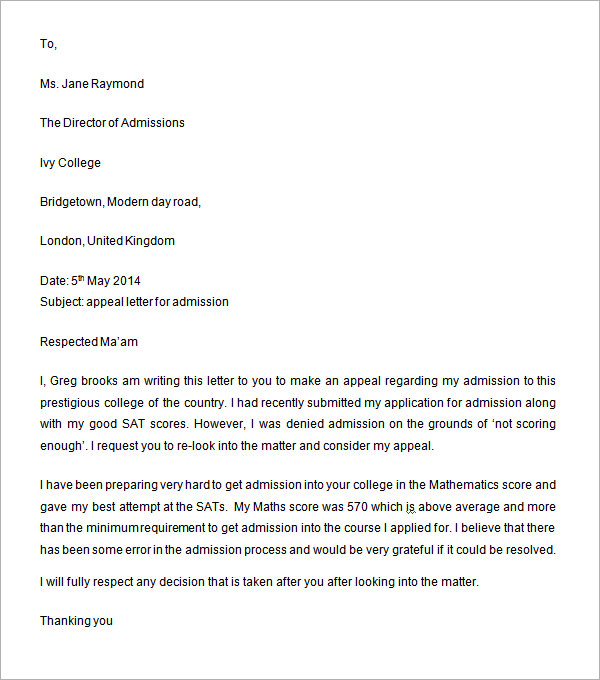
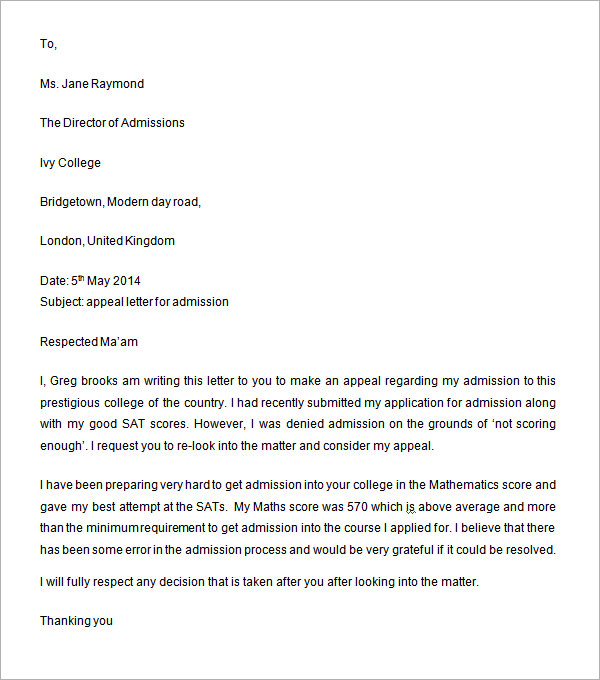
What is a sample appeal letter?
What to Include in an Appeal Letter: Step-by-Step
- Use a Professional Tone. Maintain the utmost professionalism and courteousness throughout the letter. ...
- Explain the Situation or Event. Clearly explain the situation that has occurred, focusing on the facts of what has taken place that you wish to appeal.
- Demonstrate Why It’s Wrong or Unjust. ...
- Request a Specific Action. ...
- Proofread the Letter Carefully. ...
How do you write a letter of appeal to insurance?
Writing a Health Insurance Appeal Letter (Free Sample)
- Many Procedures are Not covered by insurance. Most people expect everything to be covered after they pay the deductible, but many medical procedures are not covered by insurance.
- Customer Service. ...
- Insurance Company Rules. ...
- certified mail. ...
- Sample Health Insurance Appeal Letter. ...
How to write an appeal letter?
Tips for Writing an Appeal Letter
- Check Company Policy. Know Where to Send Your Letter. ...
- Use Business Letter Format. It is an official letter, so be sure to use proper business letter format.
- Use a Polite Tone. Try to avoid any anger or judgment in your writing. ...
- Admit Any Mistakes. ...
- Stick to the Facts. ...
- Keep it Brief. ...
- Carefully Edit Your Letter. ...
- Follow Up. ...
How to appeal health insurance claim denials?
Understand the reason for the denial. Ask that it be clearly stated in writing and that the appeal process for this particular kind of denial be made clear to you. Quite often, the insurance company appears to hope that by saying “no” and offering no further information, it can stop the conversation.
How do I write an insurance denial appeal letter?
Things to Include in Your Appeal LetterPatient name, policy number, and policy holder name.Accurate contact information for patient and policy holder.Date of denial letter, specifics on what was denied, and cited reason for denial.Doctor or medical provider's name and contact information.
How do I appeal insurance denial?
You or your doctor contact your insurance company and request that they reconsider the denial. Your doctor may also request to speak with the medical reviewer of the insurance plan as part of a “peer-to-peer insurance review” in order to challenge the decision.
How do I write a letter of appeal for medical necessity?
A medical necessity appeal letter format can be tricky. First check the patient's policy to make sure the procedure is not specifically excluded. In the letter, state the provider's name, patient's name, date of service and procedure in question. Also list the patient's identification, group, policy and claim numbers.
What do you do about the amount that the insurance company has denied?
Your right to appeal Internal appeal: If your claim is denied or your health insurance coverage canceled, you have the right to an internal appeal. You may ask your insurance company to conduct a full and fair review of its decision. If the case is urgent, your insurance company must speed up this process.
What should be included in an appeal letter?
What to Include in an Appeal Letter. In an appeal letter, you state the situation or event, explain why you think it was wrong or unjust, and state what you hope the new outcome will be. Your appeal letter is your chance to share your side of the situation.
How do you write a denial letter of claim?
What Should be in your Claim Denial Letter?Your name, position and company.The date the claim was filed.The date of your denial.The reason for the denial.The client's policy number.The claim number.
How do I write an appeal letter for reimbursement?
I appreciate the opportunity to bring this matter to your attention as a formal appeal. I hope for your reconsideration of the original claims payment and look forward to a reasonable and appropriate reimbursement payment based upon the total charges, costs, and time and work involved for a physician.
What is an example of a medical necessity?
The most common example is a cosmetic procedure, such as the injection of medications, such as Botox, to decrease facial wrinkles or tummy-tuck surgery. Many health insurance companies also will not cover procedures that they determine to be experimental or not proven to work.
How do you handle a denied medical claim?
Call your doctor's office if your claim was denied for treatment you've already had or treatment that your doctor says you need. Ask the doctor's office to send a letter to your insurance company that explains why you need or needed the treatment. Make sure it goes to the address listed in your plan's appeals process.
What are the two types of claims denial appeals?
There are typically two levels of appeal: a first-level internal appeal administered by the insurance company and then a second-level external review administered by an independent third-party.
How do you write a grievance letter to an insurance company?
How to Write a Grievance to an Insurance CompanyKnow Your Rights. Go through your policy handbook and read up on your rights as a policy holder. ... Be Specific. Be specific about everything you put in writing. ... Stick to Guidelines. ... Include Attachments. ... Make it Easy.
What happens when an insurance company denies a claim?
If your claim is denied, regardless of how valid you believe it is, you'll most likely need to hire an attorney if you choose to fight the denial. After all, insurers make a profit by taking in more money in premiums than they pay out in claims.
What is a physician's sample appeal letter?
Some physicians are far removed from the appeal process and are unsure of the specifics of your denial. They may also be unsure of the amount of information necessary. It is important that you communicate the specific reason for the denial to your treating physician and ask that they write their appeal letter with enough information to address the denial specifically.
What is the purpose of an appeal letter?
The purpose of the appeal letter is to tell the insurance company that you disagree with their decision and why you believe they should cover the procedure . The letter should be factual and written in a firm but pleasant tone. When writing your appeal letter you should include the following:
What to do if your insurance is denied?
Most plans have several levels of appeal. If your appeal has been denied, you also need a copy of the second denial letter.
What is the second level of appeal?
Typically, the second level of appeal will be reviewed by a different group of people at the insurance company. Usually, your second denial letter will explain the reason for denial and may even ask that you submit specific information that was not received with your first appeal letter.
What does it mean when your doctor says you are denied treatment?
Simply stated, a denial means that the insurance company has decided not to pay for the treatment that your doctor has recommended. The treatment may have already been performed or may be scheduled in the near future.
What is a denial letter for ERISA?
Under the Employee Retirement and Income Security Act (ERISA), your denial letter should include a specific reason for the denial and a reference to your plan explaining the basis for the denial.
Why do insurance companies deny treatment?
Often an insurance company will deny a treatment because they believe there is not enough evidence that the treatment is helpful for a specific disease. If you and your doctor believe this is the basis for your denial, you need to submit documentation that the treatment is effective.
What is a letter to insurance company?
If possible send the letter from a lawyer or a third party who acts on your behalf. This letter is written to be sent to insurance company for a coverage that was denied for a medical treatment.
How to write a letter to a patient?
Start the letter off by date, name of the insurance company and their address. Make sure to also add policyholders name, type of coverage and the patient’s policy number. As a third party, state the name of the patient and your reason for writing the letter.
Can insurance reject cancer claims?
As someone with cancer or a caregiver for someone with cancer, you have a lot on your mind without having to worry about payments and insurance. Unfortunately, some insurance companies may reject claims for certain health services. You do have the option to appeal, however.
Is name of service, procedure, or treatment sought a covered service?
[Name of service, procedure, or treatment sought] is stated as a covered benefit in your HMO Member Handbook, is implicitly covered in the Evidence of Coverage, and is not expressly excluded as a covered service in the Evidence of Coverage.
What is an insurance appeal letter?
Insurance appeal letters are meant to get the amount that has been deposited or invested in the stipulated program or any financial institution. The insurance appeal letters can be multipurpose in nature. The letter will ask for the money that is already deposited by the client when he is in need of money.
What should a letter specify?
The letter should specify the topic. The letter should specify the specifications of the scheme. If complaints, it should be addressed to the proper authority. The letter should be supported by appropriate facts and figures. The letter should contain all the information about the scheme that you have enrolled in.
What should a letter contain?
The letter should contain all the information about the scheme that you have enrolled in. The letter should specify the details of the agent, nearest branch, etc. If you have any written document in this regard either from the agent or the office, you should submit that too.
What should a letter include when a denial is filed?
Any letter written to appeal a denial should include a response to the specific reasons given for the denial. Before writing a letter you must request the reasons for denial in writing, if you have not already received this and also request copies of any plan guidelines that were used in support of the denial.
What is appeal strategy?
Appeal Strategies. The ability to make a successful clinical appeal when requested treatment services are denied by an insurer is an important skill for psychiatrist to have in today’s environment . No one strategy will prove successful at all times and in all situations; often success will lie in a combination of approaches depending on ...
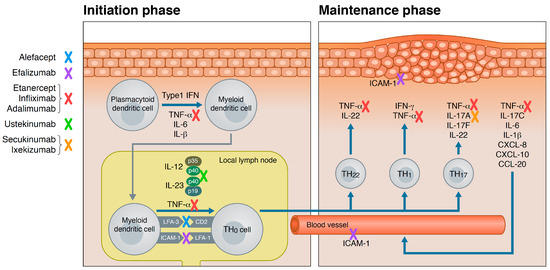
Not Medically Necessary
Experimental
Out of Network
- Try to show your plan didn’t have access to a provider with the needed specialty in-network, or there was an unreasonably long wait time for an in-network provider.
Health Care Setting
- In-home care instead of hospitalization may be covered if you show that in-home care would be less expensive and will meet the medical needs of the patient. Show that your provider recommends the best care is in-home care instead of hospitalization. Provide an in-home care treatment plan approved from your provider. Depending on the type of plan, it may help to cite st…
Policy Cancelled For Lack of Payment
- Explain why the payment wasn’t made, such as a payroll error, or a new bank account was established and you forgot to notify the insurer of the account change. Explain that you have been a customer for a long time and have always made your payments on time. Ask your insurer to make a one-time exception and reinstate your coverage.
External Review by An Independent Review Organization
- The external review is one of several steps in the appeal process when an independent third-party reviews your appeal to determine whether the insurer should cover your claim or not. It's requested after you've exhausted your insurance company’s internal review process without success. To check out other IRO decisions for health insurance appeals, use our searchable dat…
We Can Help You with Your Insurance!
- Watch a one-minute video about how our insurance experts can help you with insurance questions and problems.