
Medication
- Diabetes Complications in Dogs and Cats: Diabetes Ketoacidosis (DKA)
- Diabetic Ketoacidosis
- Diabetic Ketoacidosis Increases Risk of Acute Renal Failure in Pediatric Patients with Type 1 Diabetes
Therapy
What lab values indicate DKA? Diabetic ketoacidosis is characterized by a serum glucose level greater than 250 mg per dL, a pH less than 7.3, a serum bicarbonate level less than 18 mEq per L, an elevated serum ketone level, and dehydration.
Self-care
Normal insulin levels for non-diabetics are usually between 60 and 100 mg/dl and may rise to 140 mg/dl after eating, reports the University of California. Diabetics may have insulin levels that range from as low as 25 mlU/L at fasting to as high as 30-230 mlU/L after recent glucose administration, reports Medscape.
Nutrition
The types of insulin used for sliding scale therapy include:
- Long-acting insulin (glargine/detemir or neutral protamine Hagedorn)
- Short-acting or rapid-acting insulin (aspart, glulisine, lispro, and regular)
- Premixed insulin (a combination of long-acting and short-acting insulin)
Why are DKA patients NPO?
What lab values indicate diabetic ketoacidosis?
What are normal levels of insulin?
What are the types of insulin therapy?
Which type of insulin is given to quickly treat ketoacidosis?
INSULIN THERAPY The current recommendation is to give low-dose (short-acting regular) insulin after the diagnosis of diabetic ketoacidosis has been confirmed by laboratory tests and fluid replacement has been initiated.
Which insulin is given in emergency?
Short-acting (regular insulin) and Rapid-acting Insulins One brand of regular insulin (e.g., Humulin R, Novolin R) may be substituted for another brand of regular insulin and for rapid-acting insulins (e.g., Humalog, NovoLog, Apidra), and vice versa, on a unit-per-unit basis in emergency conditions.
What is the emergency treatment of diabetic ketoacidosis?
If you're diagnosed with diabetic ketoacidosis, you might be treated in the emergency room or admitted to the hospital. Treatment usually involves: Fluid replacement. You'll receive fluids — either by mouth or through a vein — until you're rehydrated.
What IV insulin is used for DKA?
Treatment of DKA with subcutaneous insulin Subcutaneous administration of insulin aspart19 and insulin lispro20 every 1 or 2 hours was as safe and efficient as continuous insulin infusion performed in the intensive care unit (ICU).
When do you take Humulin N?
Humulin N (human insulin) is injected underneath the skin (subcutaneously) twice per day. The number of units of insulin is different for each person.
How do you get insulin in an emergency?
If you are in emergency need of insulin right now, always go to the emergency room.If you are in emergency need of insulin right now, always go to the emergency room.At Walmart, you can buy insulin for $25 without a prescription (“over-the-counter”) and without insurance.More items...
When is DKA an emergency?
Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated immediately. Go to the emergency room or call 911 right away if you can't get in touch with your doctor and are experiencing any of the following: Your blood sugar stays at 300 mg/dL or above. Your breath smells fruity.
How is emergency hyperglycemia treated?
Emergency treatment for severe hyperglycemia Treatment usually includes: Fluid replacement. You'll receive fluids — usually through a vein (intravenously) — until you're rehydrated. The fluids replace those you've lost through excessive urination, as well as help dilute the excess sugar in your blood.
Which insulins are short acting?
Types of insulin 1TypeExamplesThe time of greatest effect (peak)Humalog ,U-200 (insulin lispro)1-3 hoursShort-actingHumulin R, Novolin ge Toronton (insulin regular)2–3 hoursIntermediate-acting14 more rows•Feb 28, 2022
When do you give Lantus to DKA?
The first Lantus insulin dose is often given at the same time as the first rapid-acting insulin dose. Although Lantus is generally given in the evening before bed (as it is a long-acting insulin), the first dose can be given as a half dose with the first meal, then the rest given that evening before bedtime.
When do you give Lantus?
Doctors typically prescribe Lantus to be used once a day, not twice a day. You can take it at any time of day, but it should be the same time every day. Most people follow a bedtime dosing schedule for Lantus.
How is insulin glargine administered?
Insulin glargine products come as a solution (liquid) to inject subcutaneously (under the skin). They are injected once a day. You should use insulin glargine products at the same time every day.
When do you give glucagon and dextrose?
Both intravenous glucagon and dextrose were effective in the treatment of hypoglycemic coma. There was a difference in the glycemic profile after intravenous glucagon compared with intravenous dextrose, and recovery of a normal level of consciousness after glucagon was slower than after dextrose (6.5 vs.
When do you give glucagon?
Your caregivers should know how to give the glucagon injection, in case your blood sugar falls too low....You need glucagon if your blood sugar level is less than 50 mg/dl and you are:Unable to eat or drink safely because you're confused or disoriented.Unconscious.Having seizures.
Is glucagon given IM or IV?
Glucagon is available for use intravenously, intramuscularly, or subcutaneously in a kit that contains a vial of sterile glucagon and a syringe of sterile diluent.
Which patient may receive insulin lispro?
In patients with type 2 diabetes, insulin lispro injection products may be used with another type of insulin or with oral medication(s) for diabetes. Insulin lispro injection products are a short-acting, manmade version of human insulin.
What is the protocol for the management of patients with DKA?
The protocol for the management of patients with DKA is presented in Figure 1. It must be emphasized that successful treatment requires frequent monitoring of clinical and metabolic parameters that support resolution of DKA (Table 1).
What are the therapeutic goals of DKA?
The therapeutic goals of DKA management include optimization of 1) volume status; 2) hyperglycemia and ketoacidosis; 3) electrolyte abnormalities; and 4) potential precipitating factors. The majority of patients with DKA present to the emergency room. Therefore, emergency physicians should initiate the management of hyperglycemic crisis while a physical examination is performed, basic metabolic parameters are obtained, and final diagnosis is made. Several important steps should be followed in the early stages of DKA management: 1 collect blood for metabolic profile before initiation of intravenous fluids; 2 infuse 1 L of 0.9% sodium chloride over 1 hour after drawing initial blood samples; 3 ensure potassium level of >3.3 mEq/L before initiation of insulin therapy (supplement potassium intravenously if needed); 4 initiate insulin therapy only when steps 1–3 are executed.
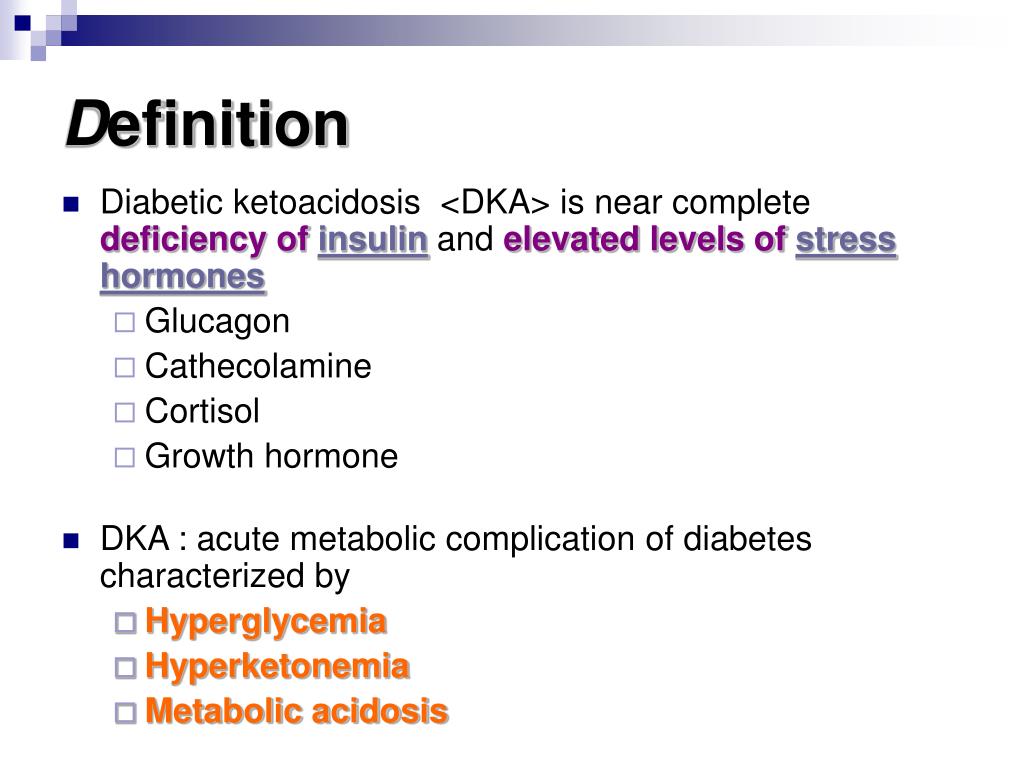
What is DKA in diabetes?
Diabetic ketoacidosis (DKA) is a rare yet potentially fatal hyperglycemic crisis that can occur in patients with both type 1 and 2 diabetes mellitus. Due to its increasing incidence and economic impact related to the treatment and associated morbidity, effective management and prevention is key. Elements of management include making the appropriate diagnosis using current laboratory tools and clinical criteria and coordinating fluid resuscitation, insulin therapy, and electrolyte replacement through feedback obtained from timely patient monitoring and knowledge of resolution criteria. In addition, awareness of special populations such as patients with renal disease presenting with DKA is important. During the DKA therapy, complications may arise and appropriate strategies to prevent these complications are required. DKA prevention strategies including patient and provider education are important. This review aims to provide a brief overview of DKA from its pathophysiology to clinical presentation with in depth focus on up-to-date therapeutic management.
How does volume resuscitation help with hyperglycemia?
Intravascular and extravascular volume resuscitation will decrease hyperglycemia by stimulating osmotic diuresis if renal function is not severely compromised and enhance peripheral action of insulin (insulin effects on glucose transport are decreased by hyperglycemia and hyperosmolarity). When glucose levels fall below 200–250 mg/dL, intravenous fluids should be switched to dextrose-containing 0.45% NaCl solution to prevent hypoglycemia, and/or insulin infusion rate should be decreased. Special considerations should be given to patients with congestive heart failure and chronic kidney disease. These patients tend to retain fluids; therefore, caution should be exercised during volume resuscitation in these patient groups. Urine output monitoring is an important step in patients with hyperglycemic crises.
How many hospitalizations for diabetic ketoacidosis in 2009?
In 2009, there were 140,000 hospitalizations for diabetic ketoacidosis (DKA) with an average length of stay of 3.4 days.1The direct and indirect annual cost of DKA hospitalizations is 2.4 billion US dollars.
Why is bicarbonate not indicated in mild and moderate forms of DKA?
Bicarbonate therapy is not indicated in mild and moderate forms of DKA because metabolic acidosis will correct with insulin therapy.3, 8The use of bicarbonate in severe DKA is controversial due to a lack of prospective randomized studies.
How much volume loss in DKA?
Fluid loss averages approximately 6–9 L in DKA. The goal is to replace the total volume loss within 24–36 hours with 50% of resuscitation fluid being administered during the first 8–12 hours. A crystalloid fluid is the initial fluid of choice.10Current recommendations are to initiate restoration of volume loss with boluses of isotonic saline (0.9% NaCl) intravenously based on the patient’s hemodynamic status.3Thereafter, intravenous infusion of 0.45% NaCl solution based on corrected serum sodium concentration will provide further reduction in plasma osmolality and help water to move into the intracellular compartment. Hyperosmolar hyponatremia due to hyperglycemia is a frequent laboratory finding in DKA and is usually associated with dehydration and elevated corrected sodium concentrations.
What is the most dangerous diabetic complication?
Diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic nonketotic coma are among the most dangerous acute diabetic complications observed in the ED. DKA is diagnosed in over 200,000 patients each year, with an increasing incidence observed between 2003 and 2014. The mainstay of treatment for DKA currently involves volume repletion with crystalloid fluids and administration of exogenous insulin to correct hyperglycemia and promote clearing or serum ketones, with the ultimate goal of correcting the anion gap acidosis. The most recent guidelines from the American Diabetes Association recommend administration of a bolus of IV insulin (0.1 U/kg) prior to starting a continuous IV insulin infusion, although it should be noted that these guidelines have not been updated since 2009 and the use of insulin bolus in adult patients with DKA has become controversial in the interim. We sought to examine the literature to determine whether there is evidence that a bolus of IV insulin prior to a continuous infusion in adult patients with DKA reduces the time to normalization of the anion gap, reduces the duration of the insulin infusion, affects length of stay, or results in increased episodes of hypoglycemia.
Can you give insulin bolus for DKA?
Unfortunately, this body of evidence is of moderate quality at best and it is difficult to strongly recommend either for or against the use of an insulin bolus for DKA in adults. While none of these studies found a clear benefit, they also not demonstrate any significant harm. It seems reasonable to omit an insulin bolus when a continuous infusion can be initiated in a timely fashion, but in cases in which the drip may be delayed, it may be prudent to give a bolus while waiting. Ultimately, the decision will need to be made on a case-by-case basis, but this limited evidence does not seem to support the routine use of an insulin bolus in these patients.
How to treat DKA?
The primary treatment is hydration, electrolyte monitoring, and insulin therapy, traditionally accomplished via IV regular insulin,. Both the American Diabetes Association (ADA) and the International Society for Pediatric and Adolescent Diabetes (ISPAD) recommend a continuous infusion of IV regular insulin as standard of care in the management of DKA. These recommendations are based primarily on studies from the 1970s ( Menzel 1970 , Fisher 1977) that suggested that the delayed onset and longer half-life of SC and IM regular insulin make these routes inadequate for the management of DKA. However, these studies evaluated the use of regular insulin, and pre-dated the development of fast-acting insulin analogs ( aspart and lispro) which may be more efficacious in the management of DKA when administered by these alternate routes. Insulin lispro, for example, has an onset of action of 10 to 20 minutes and reaches peak concentration within 30-90 minutes when administered by SC injection ( Holleman 1997 ).
How is DKA managed?
ICU admissions also drastically increase the cost of care. While patients in DKA are often critically ill, their care is generally algorithmic, and may not require ICU level care in those without severe DKA. Given that ICU care is often dictated by the use of a continuous IV infusion of insulin, an alternative regimen that involves intermittent SC insulin may allow admission to general medical wards or “step-down” units.
Is SC insulin safe for DKA?
The outcomes from these studies suggest that the use of SC fast-acting insulin is both safe and effective at treating mild to moderate DKA. No differences were observed in the duration of therapy required to resolve hyperglycemia or DKA in any of these studies. The incidence of hypoglycemia was low in the all of the studies and similar with either treatment. There were no episodes of recurrent DKA or death noted in any of the studies. An initial SC injection of 0.3 units/kg of insulin aspart or lispro can be given, followed by SC injections either hourly (0.1 units/kg) or every 2 hours (0.2 units/kg) with similar safety and efficacy to continuous IV insulin. A Cochrane systematic review and meta-analysis of this topic identified one additional study in adults ( Ersöz 2006) and one study involving pediatric patients ( Della Manna 2005 ), both of which demonstrated similar safety and efficacy.
How does insulin help with DKA?
Insulin therapy is a mainstay in the management of DKA because it reduces the production of hepatic glucose, increases the utilization of peripheral glucose and inhibits lipolysis, ketogenesis and glucagon secretion, resulting in lowering of plasma glucose and decreasing the production of ketoacidosis.[ 47] Insulin is usually given through IV route, starting with a bolus of regular insulin at a dose of 0.1 unit/kg body weight, and then, within 5 min followed by a continuous infusion of regular insulin of 0.1 unit/kg/h.[13,48] There was no difference in outcomes if IV insulin infusion is started without a bolus dose but at a higher rate of insulin at 0.14 unit/kg body weight/h.[49,50] In children, a bolus dose of insulin prior to the IV infusion is not recommended, as it does not improve clinical outcomes and may contribute to the development of cerebral edema.[45,51,52]
What is DKA in diabetes?
Diabetic ketoacidosis (DKA) is the most common hyperglycemic emergency and causes the greatest risk for death in patients with diabetes mellitus . DKA more commonly occurs among those with type 1 diabetes, yet almost a third of the cases occur among those with type 2 diabetes. Although mortality rates from DKA have declined to low levels in general, it continues to be high in many developing countries. DKA is characterized by hyperglycemia, metabolic acidosis and ketosis. Proper management of DKA requires hospitalization for aggressive intravenous fluids, insulin therapy, electrolyte replacement as well as identification and treatment of the underlying precipitating event along with frequent monitoring of patient's clinical and laboratory states. The most common precipitating causes for DKA include infections, new diagnosis of diabetes and nonadherence to insulin therapy. Clinicians should be aware of the occurrence of DKA in patients prescribed sodium-glucose co-transporter 2 inhibitors. Discharge plans should include appropriate choice and dosing of insulin regimens and interventions to prevent recurrence of DKA. Future episodes of DKA can be reduced through patient education programs focusing on adherence to insulin and self-care guidelines during illness and improved access to medical providers. New approaches such as extended availability of phone services, use of telemedicine and utilization of public campaigns can provide further support for the prevention of DKA.
What is the DKA deficit?
DKA is associated with a significant total body deficit of serum electrolytes, particularly sodium, chloride and potassium. On average, patients with DKA have the following deficits of electrolytes per kilogram of body weight: sodium, 7–10 mEq/kg; potassium, 3–5 mEq/kg and chloride, 3–5 mmol/kg.[13,37] Replacement of sodium and chloride will follow the guidelines mentioned above.
What is DKA in medical terms?
DKA is a medical emergency that requires prompt management in a hospital setting. The mainstays of its management include restoring the circulatory volume, correcting electrolyte abnormalities, treating hyperglycemia and diagnosing and treating the precipitating cause.
What should be included in a DKA test?
The initial laboratory testing should include plasma glucose, electrolytes, serum ketones (if unavailable, urine ketones can be obtained), complete blood count and initial arterial (or venous) blood gases. DKA is characterized by hyperglycemia, the presence of ketone bodies and acidosis. Plasma glucose is generally elevated to >13.9 mmol/L (250 mg/dL). However, a wide range of plasma glucose levels can be present, which is independent of the severity of DKA.[13] Normal or lower levels of glucose have been reported, a condition called “euglycemic DKA,” in about 10% of patients who present with DKA.[31] Patients who are prescribed SGLT2 inhibitor therapy may develop euglycemic DKA and the diagnosis of DKA can be missed or delayed in these cases; therefore, the physician should have a high level of suspicion when evaluating such patients.
Why is DKA important?
DKA continues to be an important cause of hospital admissions and mortality among patients with diabetes. Infections and nonadherence to insulin therapy remain the most common causes of DKA. Proper management of DKA includes prompt initiation of IV fluids, insulin therapy, electrolytes replacement and recognition and treatment of precipitating causes. Close monitoring of patient's condition by regular clinical and laboratory data and the use of management protocols help ensure better outcomes. Prevention of DKA through structured educational programs and identification of risk factors for recurrence should be part of the patient's care plan.
What is the second feature of DKA?
The second feature of DKA is the presence of ketones in the urine and/or serum. There are three types of ketones: beta-hydroxybutyrate, acetoacetate and acetone. It is recommended to measure serum beta-hydroxybutyrate (normal, <0.6 mmol/L) if urine ketones are negative when the diagnosis of DKA is suspected.[32] Point-of-care capillary beta-hydroxybutyrate measurement has been found to be both sensitive and specific for DKA when compared with ketone testing using the nitroprusside method.[33]
IN BRIEF
This article reviews the most common and immediately life-threatening diabetes-related conditions seen in hospital emergency departments: diabetic ketoacidosis, hyperglycemic hyperosmolar state, and hypoglycemia. It also addresses the evaluation of patients with hyperglycemia and no previous diagnosis of diabetes.
Hyperglycemic Crisis: DKA and HHS
DKA is responsible for > 110,000 hospitalizations annually in the United States, with mortality ranging from 2 to 10%. 7 – 9 HHS is much less common but confers a much greater mortality. 10 In both diseases, mortality is largely related to underlying comorbidities such as sepsis. 11
Clinical presentation
DKA and HHS are characterized by absolute or relative insulin deficiency, which prevents the body from metabolizing carbohydrates and results in severe hyperglycemia. As blood glucose levels rise, the renal glucose threshold is overwhelmed, and urine becomes more dilute, leading to polyuria, dehydration, and polydipsia.
Initial evaluation
Patients with severe hyperglycemia should immediately undergo assessment and stabilization of their airway and hemodynamic status. Naloxone, to reverse potential opiate overdose, should be considered for all patients with altered mentation.
Intravenous Fluid
Critically ill patients with severe hyperglycemia resulting from DKA or HHS should be treated immediately with a bolus of normal saline.
Insulin therapy
Critically ill patients with DKA should be given a loading dose of regular insulin at 0.1 units/kg body weight to a maximum of 10 units followed by an infusion of regular insulin at 0.1 units/kg body weight/hour, to a maximum of 10 units/hour.
Electrolyte replacement
Patients with DKA or HHS experience rapid shifts in potassium during resuscitation that may trigger life-threatening arrhythmias. Death during initial resuscitation of patients with DKA is usually caused by hyperkalemia, whereas hypokalemia is the most common cause of death after treatment has been initiated.
What should be included in a DKA workup?
DKA work-up should include CBC, electrolytes, extended electrolytes, creatinine, BUN, albumin, VBG, lactate, serum ketones, as well as consideration for: Lactate is a potentially important prognostic factor in predicting the severity of DKA and in monitoring the progression or resolution.
What is euglycemic DKA?
Euglycemic DKA involves a relative carbohydrate deficiency state/normalization of serum glucose and concomitant elevation of counter-regulatory stress hormones that leads to free fatty acid catabolism and ketone production.
Why is DKA a precipitating cause?
Most often, it is due to medication non-adherence, incorrect dosing or infection.
Why is potassium high in DKA?
However, the initial potassium reading is commonly normal or high due to intracellular shifts secondary to volume contraction and metabolic acidosis. Potassium must be replaced prior to initiation of insulin therapy as insulin further promotes an intracellular shift of potassium.
When to add dextrose to IV fluid?
Add dextrose (D5W) to the IV fluid if/when blood glucose approaches normal to allow continued insulin infusion at a rate sufficient to resolve DKA while avoiding hypoglycemia OR when glucose <15 (250-300mg/DL) switch to D5-1/2NS NS at an initial rate of 150 to 250 mL/h
How to avoid cerebral edema in the management of DKA?
The key to avoiding cerebral edema in the management of DKA is to go slow with resuscitation.
What drugs can trigger DKA?
In addition, common drugs that can trigger DKA include glucocorticoids, diuretics and atypical antipsychotics.
What is the primary problem with DKA?
The primary problem with DKA is ketoacidosis (not hyperglycemia). Therefore, our overall goal is to titrate insulin as needed to treat the ketoacidosis (figure above).
What causes DKA in a patient?
However, DKA can be caused by any source of physiologic stress. Occasionally, DKA is the presentation of a serious underlying problem, such as occult sepsis. Common causes of DKA include: Insulin non-adherence, inadequate dosing, or insulin pump failure.
Why is DKA so depleted?
DKA patients are often profoundly volume depleted (e.g., due to vomiting, reduced oral intake, and osmotic diuresis). Hypovolemia triggers the release of stress hormones (e.g., catecholamines, cortisol) which cause insulin resistance and thereby exacerbate the DKA. So prompt reversal of hypovolemia is important.
What is the gold standard for defining the presence and extent of ketoacidosis in DKA?
Beta-hydroxybutyrate level is the gold standard for defining the presence and extent of ketoacidosis in DKA.
What pH level is ketoacidosis?
Some patients will present with profound ketoacidosis (e.g. pH<6.9 or bicarb <5 mM). Patients generally tolerate this surprisingly well.
Why is hypokalemia so bad?
Hypokalemia is extremely problematic, because insulin cannot be given to patients with significant hypokalemia ( since insulin will exacerbate the hypokalemia). Thus, hypokalemia impairs our ability to treat DKA.
Why is dextrose added to IV fluid?
As the glucose falls, dextrose must be added to the IV fluid to allow for ongoing insulin administration (since ongoing insulin administration is needed to correct the ketoacidosis).
What is the common mistake in the management of DKA?
One common mistake in the management of DKA is premature discontinuation of the insulin infusion (either accidentally or in a misguided attempt to manage hypoglycemia). This may cause rapid widening of the anion gap.
When should basal insulin be given?
There is no necessity to provide basal insulin immediately upon admission. Ideally, basal insulin should be provided well in advance of discontinuation of the insulin infusion (e.g. >4 hours before) to facilitate a smooth transition.
How long does it take to get insulin infusion?
Then the provider will first order long-acting insulin from pharmacy. Subsequently, after the long-acting insulin arrives and is administered, the insulin infusion can be stopped two hours later. The process of ordering long-acting insulin, receiving it from pharmacy, and then waiting two hours takes about three hours.
How long does it take for basal insulin to peak?
Newer types of basal insulin (especially detemir) may take more than two hours to reach peak effect.
How many doses of glargine are needed for a patient on insulin?
For patients are on twice-daily glargine, this will include two doses of glargine. For patients on an insulin pump, the basal insulin can be calculated by integrating the basal rate of insulin over a 24-hour period (of course, in such patients, the pump should be discontinued).
Is basal insulin a once daily insulin?
The full dose of basal insulin should be provided in the form of a once-daily insulin dose (e.g. glargine or detemir). Administration of reduced doses will lead to confusion subsequently, as it will be unclear whether the patient has received basal insulin.
Is basal insulin safe?
However, it does support the idea that early home-dose basal insulin is safe and feasible. We have continued to have favorable results with this, which remains our routine practice today.
