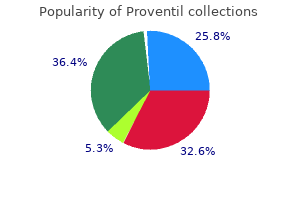
Approximately 20% of patients deferred therapy, particularly in community-based treatment centers. Receipt of treatment was not associated with any patient sociodemographics. Management patterns for elderly patients with AML have been changing with the introduction of novel targeted therapies and hypomethylating agents.
Full Answer
Why is it so difficult to treat the elderly?
The decision to treat—or not treat—an older patient may be difficult; aging is highly individualized so treatment decisions cannot be made on the basis of age alone. And because the elderly are under-represented in clinical trials, information about how to best treat an older population is limited.
Should hospitalists help seniors reassess medication regimens?
But she adds that hospitalists have an excellent opportunity to help elderly patients reassess their medication regimens precisely because they are new to the patient. “When a patient is unknown to a physician in the hospital, that’s an opportunity to revisit everything freshly and to avoid what we call clinical inertia,” Dr. Holmes says.”
When is it necessary to treat a patient who refuses treatment?
It may also be necessary to treat patients who refuse treatment in emergencies where capacity is likely to be impaired but there is not sufficient time for its assessment. What legal frameworks are currently in use?
Do geriatric patients have the right to refuse treatment?
The American Hospital Association and the U.S. Supreme Court have each delineated certain rights to which patients who have the competence and mental capacity to make decisions for themselves are entitled. One such right especially important to geriatric patients is the right to refuse treatment.

What do you do when someone refuses medical treatment?
What to Do if Your Loved One Refuses to See a DoctorBe transparent and direct. ... Convince them that it's their idea. ... Make it a "double-checkup" ... Make the rest of the day as enjoyable as possible. ... Get someone who is an authority figure to help.
What are some factors that may complicate the treatment regimen for older adults?
Among them are an older age, a low level of education, the possibility of side effects during pharmacotherapy, problems with memory or poor cognition, low socioeconomic status (unaffordability of medications), and the lack of proper instruction on the use of medicines from the health care professionals.
What are a few examples of when a patient can refuse treatment?
1 Accordingly, the patient may refuse to be informed about their medical condition and make a decision. An example would be the statement, “I don't want to hear anything from you. I'm not going to the hospital.” They may be informed and then refuse to make a decision. “Wow, that sounds bad either way.
Why would a patient refuse treatment?
Explore Reasons Behind Refusal Patients may refuse treatments for many reasons, including financial concerns, fear, misinformation, and personal values and beliefs. Exploring these reasons with the patient may reveal a solution or a different approach.
What are some of the reasons for lack of adherence to depression treatment in older adults?
Predictors of treatment non-adherence among young and older adults with depressionIllness beliefs. ... Treatment beliefs. ... Self-stigma and perceived stigma. ... Self-esteem.
Why do elderly stop taking medication?
This may be because changes in depression, health and communication in effect at six months led to long-term behavior changes. Short-term improvements in depression and self-reported health were associated with long-term changes in medication adherence among subjects who reported major depression symptoms at baseline.
When you encounter a patient who refuses treatment you should?
When you encounter a patient who refuses treatment, you should: inform the patient of the consequences of that decision.
What 3 elements must a patient demonstrate in order for a refusal to be lawful?
3) In order for a patient to refuse treatment and/or transportation two events must occur to protect both the patient and yourself: 1) You must give the patient enough information about the decision Page 2 2 they are making so that there is an informed consent, and; 2) You must be satisfied that the patient has ...
What should a nurse do if a patient refuses treatment?
If your patient refuses treatment or medication, your first responsibility is to make sure that he's been informed about the possible consequences of his decision in terms he can understand. If he doesn't speak or understand English well, arrange for a translator.
What is the term called when a patient refuses treatment?
Informed refusal is where a person has refused a recommended medical treatment based upon an understanding of the facts and implications of not following the treatment. Informed refusal is linked to the informed consent process, as a patient has a right to consent, but also may choose to refuse.
Why is refusal of treatment an ethical dilemma?
In general, ethical tension exists when a physician's obligation to promote a patient's best interests competes with the physician's obligation to respect the patient's autonomy. “When you don't take your medication, you're more likely to get sick.”
Can a competent patient refuse life-sustaining treatment?
Similarly, if the patient refusing the life-sustaining treatment is competent, one of the two necessary conditions for treatment discussed above is not fulfilled and hence the patient's health care providers are not ethically permitted to start the treatment.
What is the starting point of treatment decisions?
This decision-making can be an ethical dilemma; however, the starting point is considering the patient’s wishes after providing accurate information about risks and benefits of treatment.
How many people are 80 and older?
According to the Census Bureau, 5.7 million people in the United States are aged 80-84 and 5.5 million are aged 85 and older. People are now living longer than ever before. In fact, the Hallmark Cards Company sells 85,000 “Happy 100th Birthday!” cards each year.
Is it difficult to suggest no treatment?
It appears it is just too difficult to suggest no treatment . The hesitation may be that no treatment is equated to “doing nothing,” which is not the case. When clinicians are fully informed about and comfortable with the principles of palliative care, there is much that can be done in the absence of cancer treatment.
Is cancer a problem for older people?
The numbers are growing, and with increasing age, come increasing medical problems. It’s not uncommon for an older patient to have heart disease, diabetes, arthri tis, and other medical disorders in addition to cancer.
Why are elderly people more likely to have more than one doctor?
Over treatment is a persistent problem among the aging population. Elderly people commonly have multiple medical issues and therefore are more likely to have more than one doctor involved in their medical care. Research shows that the more doctors an individual has, the more likely they are to be prescribed conflicting medications and undergo unnecessary procedures. The problem is that, for elderly people, unnecessary tests and surgeries can have dire consequences.
Do doctors give complete information about treatment plans?
However, it often falls to patients and their caregivers to ask questions and gain a thorough understanding of their medical options. Doctors may not always provide complete information about a treatment plan voluntarily, and they may not be aware of what each patient’s goals and concerns are.
Can you feed someone with dementia?
For people with severe dementia who can no longer eat on their own, percutaneous feeding tube s are sometimes recommended to ensure adequate nutrition and avoid aspiration. However, the AGS, the AMDA and the American Academy of Hospice and Palliative Medicine (AAHPM) all caution against the insertion of feeding tubes for patients in the later stages of dementia. Instead, they suggest oral assisted feedings as the preferable option. “Contrary to what many people think, tube feeding does not ensure the patient’s comfort or reduce suffering; it may cause fluid overload, diarrhea, abdominal pain, local complications, less human interaction and may increase the risk of aspiration,” according to the AMDA.
Can dementia cause dizziness?
Medical professionals and elder care experts have hotly debated the effectiveness of these drugs, trying to tease out the specific benefits for people with dementia and weigh them against the side effects, which can include confusion, incontinence, dizziness and even an increased risk of sudden death.
Can you take risperidone with dementia?
Both the AGS and the AMDA advise that antipsychotic medications, such as quetiapine (Seroquel), risperidone (Risperdal) and olanzapine (Zyprexa), should not be given to people with dementia unless other nonpharmacologic methods of managing anxiety and dementia-related behaviors have already been attempted. “Antipsychotic medicines are often prescribed, but they provide limited benefit and can cause serious harm,” says the AGS in a statement. The effectiveness of these prescriptions vary, depending on the individual and the type of dementia they have. Medical professionals and elder care experts have hotly debated the effectiveness of these drugs, trying to tease out the specific benefits for people with dementia and weigh them against the side effects, which can include confusion, incontinence, dizziness and even an increased risk of sudden death.
What journal did the report on the withdrawn treatment of a patient come from?
The report's findings were published in the Journal of Medical Ethics, the official journal of the Institute of Medical Ethics. Researchers found that treatment was withdrawn or withheld in 37% of the cases sampled.
Is it important to protect the elderly from rash decisions?
While there will always be competing opinions on how to end someone's life with dignity, protecting the elderly from rash decisions during end-of-life care has always been a top priority in the medical community. Even if the data shows that physicians are withholding or withdrawing treatment from older patients more often than younger ones, ...
When can MCA be used?
Summary points. Common law can be used to treat patients in emergencies, especially when the diagnosis is unclear. It allows necessary and proportionate restraint until Mental Capacity Act (MCA) or Mental Health Act (MHA) assessments are completed. The MCA can be used to restrain and treat patients without capacity (for a specific decision) ...
When acting against a patient's wishes, is the MCA used?
As a general rule, when acting against a patient’s wishes, the MCA is used to treat physical disorders that affect brain function and the MHA is used to treat primary mental (psychiatric) disorders. In part two of the case scenario the patient’s behaviour has changed.
What is the first step in a mental health case?
The first is to determine the urgency of treatment to see whether common law is applicable. The second is to determine what is being treated—a primary physical (organic) disorder or a primary mental (psychiatric) disorder. We will now explain how to work through these two steps as we look at the evolving case scenario.
Can patients be treated against their wishes?
Patients can be treated against their wishes only if their decision making capacity is impaired and if the proposed treatment is for something serious enough to warrant over-riding their wishes.
Can a section 5 order be used in an outpatient setting?
The patient is already admitted: a section 5 (2) order can be used only in the inpatient setting (but not emergency or outpatients departments, although in some trusts or health boards the clinical decisions unit may count as an inpatient setting)
Can a delirium patient use the MCA before the MHA?
Where possible, the MCA should be used before the MHA. In this case, it would also be appropriate to use the MHA to keep the patient on the ward to treat his mental disorder. If he refused treatment, ongoing treatment of his physical health conditions (femoral and pelvic fracture) would need to take place within the framework of the MCA.
Why is the selection of therapy in older patients more complex?
As discussed, the selection of therapy in older patients is more complex because they are more likely to have coexistent health conditions that affect organ function and the ability to tolerate treatment. Establishing the goals of treatment is the first step in therapy selection ( Figure 1 ).
Is there a single treatment regimen for CLL?
The fact that a majority of CLL patients have comorbid conditions and greater than half have at least one major comorbidity underscores that therapy selection must be individualized. There is unlikely to be a single treatment regimen that will be an optimal fit for all older patients.
What percentage of Americans have delayed or avoided medical care?
What is added by this report? By June 30, 2020, because of concerns about COVID-19, an estimated 41% of U.S. adults had delayed or avoided medical care including urgent or emergency care (12%) and routine care (32%). Avoidance of urgent or emergency care was more prevalent among unpaid caregivers for adults, persons with underlying medical ...
How many people have delayed medical care in 2020?
As of June 30, 2020, an estimated 41% of U.S. adults reported having delayed or avoided medical care during the pandemic because of concerns about COVID-19, including 12% who reported having avoided urgent or emergency care.
Does delay in medical care increase morbidity?
However, medical care delay or avoidance might increase morbidity and mortality risk associated with treatable and preventable health conditions and might contribute to reported excess deaths directly or indirectly related to COVID-19 ( 2 ). To assess delay or avoidance of urgent or emergency and routine medical care because ...
Who is more likely to avoid urgent care?
Avoidance of urgent or emergency care was more prevalent among unpaid caregivers for adults, persons with underlying medical conditions, Black adults, Hispanic adults, young adults, and persons with disabilities.
Does delay in care increase risk?
In contrast, delay or avoidance of care might increase risk for life-threatening medical emergencies. In a recent study, states with large numbers of COVID-19–associated deaths also experienced large proportional increases in deaths from other underlying causes, including diabetes and cardiovascular disease ( 7 ).