Treatment responses are prompt compared with other standard therapies: 50% show MDD response in the first week and 50% exhibit MDD remission within 2 weeks from ECT (4). However, data are limited for patients with concurrent medical conditions, let alone life-limiting illness.
Full Answer
What happens after ECT treatment?
· In a recent large study carried out by the Consortium for Research in ECT (CORE), Husain and colleagues 3 reported that 34% of 253 patients achieved remission (HAM-D score of 10) at or before the 6th session with ECT (within 2 weeks) and 65% achieved remission at or before the 10th session (within 3 to 4 weeks).
What is the difference between electroconvulsive therapy (ECT) and ongoing treatment?
· ECT may cause memory loss and confusion. Your confusion may go away in a short time, such as 1 hour after your treatment. You may lose your memory for 1 to 3 weeks, and some memories may be lost forever. You may also get a headache after an ECT treatment. These headaches usually only last a short time.
Is ECT safe and effective?
Electroconvulsive therapy (ECT) is a medical procedure that involves passing a mild electric current through your brain, causing a short seizure. This procedure is proven to have strong positive effects on severe, treatment-resistant mental health conditions. ECT’s history stretches back more than 80 years, and extensive research shows it’s ...
How long does it take to wake up after ECT?
· One study indicated that for bipolar depression, ECT offers a fast response, usually within several weeks. Some studies indicate it can take up to six treatments to start seeing results. However, ECT usually responds more quickly than the time it takes medications, such as antidepressants, to begin fully working.
How long does it take for ECT to start working?
Results. Many people begin to notice an improvement in their symptoms after about six treatments with electroconvulsive therapy. Full improvement may take longer, though ECT may not work for everyone. Response to antidepressant medications, in comparison, can take several weeks or more.
How soon after ECT Do you feel better?
Medications typically take up to eight weeks to show improvement. “With ECT, I can get them feeling better in two weeks or less,” said Weeks. It can also be very effective in patients for whom multiple medications have failed.
How long do the effects of electroconvulsive therapy last?
There is considerable variability in the trajectories, but most commonly there is progressive symptomatic improvement within the first week and complete remission within 3 to 4 weeks.
How long does it take for memory to come back after ECT?
The most persistent adverse effect is retrograde amnesia. Shortly after ECT, most patients have gaps in their memory for events that occurred close in time to the course of ECT, but the amnesia may extend back several months or years. Retrograde amnesia usually improves during the first few months after ECT.
Can you feel worse after ECT?
ECT can't prevent future depression, or fix any ongoing stresses or problems that are contributing to how you're feeling. Some people have very bad experiences of ECT, for example because they feel worse after treatment or are given it without consent. You might not want to risk the possibility of getting side effects.
How many ECT treatments can a person have?
People undergoing ECT need multiple treatments. The number needed to successfully treat severe depression can range from 4 to 20, but most people need a total of 6 to 12 treatments. The treatments are usually given three times a week — Monday, Wednesday, and Friday.
Can ECT reset your brain?
ECT has been referred to as a “reset button for the brain,” which not only directly improves depressive symptoms, but also allows current medications to work more effectively.
What happens if ECT doesn't work for depression?
If nothing else has helped, including ECT, and you are still severely depressed, you may be offered neurosurgery for mental disorder (NMD), deep brain stimulation (DBS) or vagus nerve stimulation (VNS).
Are you tired after ECT?
You may experience other side effects immediately after treatment. These can include: drowsiness (you may sleep for a while) confusion.
Does ECT destroy brain cells?
Other findings indicate that the passage of electricity, thermal effects, and the transient disruption of the blood-brain barrier during ECS do not result in structural brain damage. Conclusions: There is no credible evidence that ECT causes structural brain damage.
Can ECT change your personality?
ECT does not change a person's personality, nor is it designed to treat those with just primary “personality disorders.” ECT can cause transient short-term memory — or new learning — impairment during a course of ECT, which fully reverses usually within one to four weeks after an acute course is stopped.
Does ECT lower IQ?
However, former patients have publicly testified that ECT can result in a very significant (>30 point) permanent decrement in IQ score (Food and Drug Administration, 1982; Andre, 2001; Cott, 2005: p.
How long does it take to respond to ECT?
We know that depressed patients often begin to respond after the first treatment and progress to wellness with 6 to 12 treatments. There is considerable variability in the trajectories, but most commonly there is progressive symptomatic improvement within the first week and complete remission within 3 to 4 weeks.
How powerful is the first ECT?
The first ECT in a series is particularly powerful. Data from the CORE study that compared right unilateral, bifrontal, and bilateral electrode placements showed that there was a 10.6 (± 8.6) HAM-D point reduction, on average, after the first ECT session (R Knapp, study statistician, personal communication, 2009). This reduction in symptoms after a single ECT session represented approximately 48% of the ultimate total decline in HAM-D scores for the full course of ECT. Symptom improvement after 1 treatment was similar for all 3 electrode placements.
Is antidepressant medication ineffective?
When a patient is urgently ill (eg, suicidal, catatonic, malnourished), this feature of the treatment may be lifesaving. Antidepressant medication may be ineffective and/or have a considerably longer lag time before symptom improvement than ECT.
Do bipolar patients need ECT?
There is evidence to demonstrate that, overall, bipolar patients require fewer ECT sessions than unipolar patients. 11 Investigation of the rapid antidepressant action of the intravenous anesthetic ketamine may lead to elucidation of related mechanisms of recovery from severe affective illness. 12.
Do patients look good after ECT?
Unfortunately, patients who have considerable symptom improvement after the first ECT session and who would be expected to do very well, never look as good as they did after that first treatment. The reasons underlying such a trajectory of symptom persistence are not yet understood.
Is electroconvulsive therapy effective?
The overall effectiveness of electroconvulsive therapy (ECT) is well known, but its speed of action is much less talked about. Here I review what is known about the time course of action of ECT in depression. Most patients who are referred for ECT have been ill with severe mood disorders for many months, some even for years.
What does the speed of response tell us about the mechanisms of action of ECT?
What does the speed of response tell us about the mechanisms of action of ECT? Clearly, in certain patients, the neurobiological changes induced by ECT include almost immediate alterations in brain systems that regulate mood and affect. Perhaps a “switch” mechanism (similar to that seen in bipolar patients) occurs; however, there is no evidence to suggest that very rapid improvement with ECT is associated with bipolar rather than unipolar depression. There is evidence to demonstrate that, overall, bipolar patients require fewer ECT sessions than unipolar patients. 11 Investigation of the rapid antidepressant action of the intravenous anesthetic ketamine may lead to elucidation of related mechanisms of recovery from severe affective illness. 12
How long does it take for ECT to go away?
ECT may cause memory loss and confusion. Your confusion may go away in a short time, such as 1 hour after your treatment. You may lose your memory for 1 to 3 weeks, and some memories may be lost forever.
What is ECT therapy?
WHAT YOU NEED TO KNOW: Electroconvulsive therapy (ECT) is a treatment that sends a small electric current to your brain to cause a seizure. The seizure affects the chemicals in your brain, which may make your brain cells work better.
Can you get a headache after ECT?
You may also get a headache after an ECT treatment. These headaches usually only last a short time. If you have a headache after ECT, ask your healthcare provider for medicine to make it go away. If more ECT treatments are planned for you, ask the healthcare provider to give you medicine before the treatments to help prevent headaches.
What is ECT?
Electroconvulsive Therapy (ECT) is a depression treatment that involves the stimulation of the brain with a controlled electrical current.
What Does ECT Treat?
ECT treats severe resistant depression and although it is exactly unclear to scientists and researchers how ECT is so effective, it has proven to be quite effective.
How Effective is ECT for Depression?
Over the past 2 or 3 decades, research has shown that about 47% to 75% of patients who have undergone the procedure have fully recovered from their depressive symptoms.
Side Effects of ECT
Electroconvulsive Therapy is a generally safe treatment for depression but like every other treatment, there are a few side effects.
ECT vs Other Treatment Options That Work
Depression is one of the easiest mental illnesses to tackle today because there are many treatment options.
How We Can Help You
TMS is the future of depression therapy and we are excited to be a part of this movement.
How long does it take for ECT to work?
Generally, symptoms start to improve after two sessions. The treatment should be stopped as soon as the person has responded adequately, if there are adverse effects, or if he/she withdraws consent. It is not understood exactly how ECT works to treat depression and the outcomes may vary from person to person.
How long does it take to wake up after ECT?
The person wakes up five to 10 minutes after treatment and is usually clear headed within 30 minutes. Often, people do not clearly recall the time around the ECT treatment and, at first, may have little memory about the period of illness around the treatment. Often, memory of these events gradually returns (see below for more information on side-effects).
How long does memory last after ECT?
Most research demonstrates that memory loss is very restricted and usually temporary. However, memory changes may last for some weeks after treatment and a few people experience long-term or even permanent loss of memories. People differ in the amount of memory loss they report from ECT and how they feel about it. The more treatments a person has, the greater the effect on their memory and, if the ECT is bilateral rather than unilateral, is likely to affect a person’s memory more as well. While some people find ECT to be a beneficial and lifesaving treatment, others find their memory loss distressing and for them, this outweighs any benefit from ECT.
How long does it take for memory loss to go away?
Generally, these resolve within a few hours, although some memory loss may persist.
Is it safe to use an ECT?
Like any procedure involving an anaesthetic, ECT involves this small amount of risk, but overall, it is regarded as a very safe treatment. Despite the myths about ECT causing brain damage, MRI studies have shown that it does not change the brain anatomy in any way, as the strength of the electrical current is too low to harm brain tissue.
How long after ECT can you drive home?
If ECT is done on an outpatient basis, a family member or friend must drive the person home after the procedure (driving is not allowed in the 24 hours following an ECT session) and stay until he or she goes to sleep that night.
What is the procedure for ECT?
Before the ECT procedure, the person is given a general anaesthetic and a muscle relaxant. Electrodes are placed on one (unilateral) or both (bilateral) sides of the scalp and a small electric current is passed between these until a brief generalised seizure occurs. The person does not feel anything due to the anaesthetic, and does not convulse due to the muscle relaxant.
What is ECT therapy?
“Electroconvulsive therapy, or ECT for short, is a treatment that involves sending an electric current through your brain, causing a brief surge of electrical activity within your brain (also known as a seizure). ” (Mind 2019)
What are the two types of ECT?
There are two types of ECT; unilateral and bilateral.
Is ECT helpful to everyone?
ECT isn’t helpful to everyone. Some people will have it and feel no difference whatsoever. Others may have it and suffer side effects that outweigh the benefits and choose not to continue. Everyone is unique and what works for one person doesn’t necessarily work for another.
Does ECT affect memory?
One of the common side effects of ECT, which a lot of people understandably worry about is memory loss. I don’t think my memory has been impacted by having ECT. It was already slightly off from years of long, recurring depressive episodes. I haven’t noticed it getting any worse since the treatment.
Can you eat after midnight?
No eating or drinking after midnight the night before ( sips of water are allowed).
When is a mood and memory assessment done?
Mood and memory assessments. These are done a few days before the first procedure and then weekly until the end of the treatments. This is so the team can keep track of changes in mood, suicidality and also monitor effects on memory and cognition.
Is there still controversy surrounding ECT?
Trust me when I say it’s come a long way from the way they used to practice it back in the day. There is however still a lot of controversy surrounding ECT because of its dark history and potential side effects. If you’re interested in the history and controversy surrounding ECT then you’ll find an abundance of material online.
What is ECT treatment?
Summary: ECT is an efficacious treatment of psychiatric disorders such as MDD or catatonia. Though substantial gaps exist in the medical literature about its use for seriously ill patients, it can be considered for those who have responded to ECT previously.
How does an ECT procedure work?
ECT Procedure: An anesthetist induces unconsciousness using a short-acting IV agent (e.g., methohexital, propofol) followed by a muscle relaxer (often succinylcholine). Bag mask ventilation is utilized while continuous EKG and pulse oximetry is monitored – intubation is usually not needed. Once unconscious and paralyzed, the psychiatrist places electrodes on the patient’s scalp and current are delivered. Seizure activity is monitored via motor activity or EEG; most seizures last 20-60 seconds. After the seizure ceases or is aborted, the patient is ventilated until the anesthetic wears off, then monitored until fully awake (1,3). Induction usually involves 2-3 treatments per week, then is tapered based on treatment response. While usual treatment courses span several weeks to months, treatments can be modified for patients with limited prognoses; even single treatments have been shown in case reports to have antidepressant effects or help to lyse catatonia within a day after treatment (2,3).
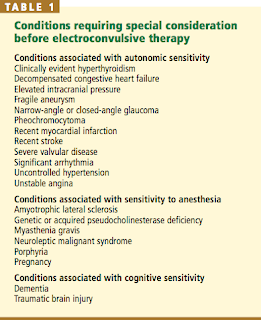
Is electrical current a contraindication?
Contraindications: While there are no absolute contraindications, the application of electrical current, production of a motor seizure, and the resultant physiological effects (e.g. transient bradycardia from vagal stimulation with subsequent sympathetic compensation leading to tachycardia) could negatively affect those with intracranial lesions; increased intracranial pressure; skull defects such as craniectomy; a recent intracranial hemorrhage or stroke; unstable angina or a recent myocardial infarction; decompensated heart failure; unstable cardiac arrhythmias; and/or unstable spinal fractures (3,5). These limitations unfortunately limit the utility of ECT for many patients with life-limiting illnesses.
What are the indications for ECT?
Indications: MDD, bipolar depression, catatonia, and refractory psychosis are the most common indications for ECT (3). There is also supporting evidence for neuroleptic malignant syndrome, status epilepticus, and Parkinson disease (3). Treatment responses are prompt compared with other standard therapies: 50% show MDD response in the first week and 50% exhibit MDD remission within 2 weeks from ECT (4). However, data are limited for patients with concurrent medical conditions, let alone life-limiting illness. Any consideration of ECT for patients with a serious illness should include a transparent acknowledgement of these limitations in the evidence. If the patient has previously responded to ECT, if symptoms are severe (e.g., high suicide risk, dangerous lack of self-care from mental illness), and/or if standard medication therapy are ineffective or not acceptable, then a psychiatry referral for evaluation for ECT should be considered (1,2). Based on case reports and practical considerations, patients with prognosis estimated in months with a fair functional status stand to gain the most quality of life benefit from ECT. Short courses (e.g., three treatments within a week) or a single treatment can be considered in cases with a prognosis of weeks.
What is the treatment for mood disorders?
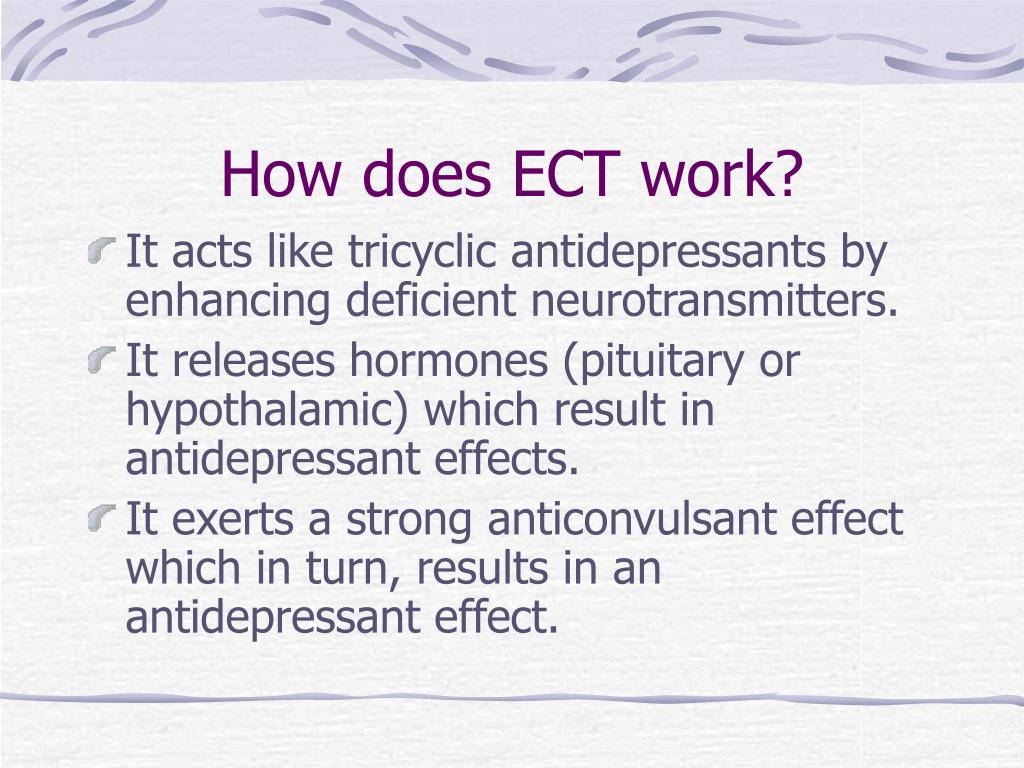
Delayed responses and marginal efficacy of many psychiatric medications pose an obstacle in alleviating suffering. Electroconvulsive therapy (ECT), a method of inducing a generalized seizure via application of electrical current to the brain, is one of the most effective treatments for MDD. Despite a paucity of evidence for use in patients with serious illness, ECT may play a select role in this population (1,2). This Fast Fact offers a primer on ECT for clinicians who commonly care for patients with severe medical illness and comorbid psychiatric disorders.
Is fast facts medical advice?
Disclaimer: Fast Facts and Concepts provide educational information for health care professionals. This information is not medical advice. Fast Facts are not continually updated, and new safety information may emerge after a Fast Fact is published. Health care providers should always exercise their own independent clinical judgment and consult other relevant and up-to-date experts and resources. Some Fast Facts cite the use of a product in a dosage, for an indication, or in a manner other than that recommended in the product labeling. Accordingly, the official prescribing information should be consulted before any such product is used.
