Physical therapy might stop if the patient isn’t seeing results or making progress within the time-frame their physical therapist thinks they should be. After all, it can be frustrating to attend regular appointments, perform all the instructed exercises and still not make progress toward your goals.
Full Answer
Can physical therapy help with DVT?
Those who are immobile for some time, such as after bed rest or failing to move after surgery, are more likely to experience DVT. If you have been diagnosed with condition or even required surgery to remove a blood clot, your physician may recommend physical therapy to improve circulation in your deep veins and prevent another episode.
When should physical therapists establish the likelihood of lower extremity DVT (Le DVT)?
Physical therapists should establish the likelihood of LE DVT when the patient has pain, tenderness, swelling, warmth, or discoloration in the lower extremity. (Evidence Quality: II; Recommendation Strength: B–Moderate) Aggregate Evidence Quality: Level II Benefit: Early intervention and prevention of adverse effects of LE DVT
How to prevent deep vein thrombosis (DVT) recurrence?
To prevent DVT recurrence, the application of graduated compression stockings is recommended "beginning within 1 month of diagnosis of proximal DVT and continuing for a minimum of 1 year after diagnosis". Physical therapists work with patients at risk for and with diagnosed DVT across the continuum of care.
Why is DVT prophylaxis so often not done?
Despite countless guidelines and education of healthcare workers, DVT prophylaxis is often not done. The fact is that DVT is preventable in the majority of patients, and the onus is on healthcare workers to be aware of the condition.
When can I resume physical therapy after DVT?
Kiser and Stefans, in 1997, conducted a retrospective case-control study and concluded that “at least 48 to 72 hours of bed rest would be prudent before return to mobilization.”14(p944) They identified 190 patients discharged from a rehabilitation facility with a diagnosis of DVT or PE.
Can I do physical therapy with DVT?
When a patient has a recently diagnosed LE DVT, physical therapists should initiate mobilization when therapeutic threshold levels of anticoagulants have been reached. Physical therapists should recommend mechanical compression (eg, IPC, GCS) when a patient has an LE DVT.
Should you Mobilise with a DVT?
For patients with a lower extremity DVT and who are at therapeutic levels for anticoagulants, the guidelines recommend that physiotherapists should initiate mobilization of the patient. The authors assessed this as a strong recommendation based on high-quality evidence.
Should PTs with DVT walk?
Conclusions: Early walking exercise is safe in patients with acute DVT and may help to reduce acute symptoms. Exercise training does not increase leg symptoms acutely in patients with a previous DVT and may help to prevent or improve the postthrombotic syndrome.
How long is bed rest for DVT?
In several countries of central Europe, patients with acute proximal deep vein thrombosis (DVT) are treated not only by anticoagulation and compression therapy but additionally by strict bed rest for 6-8 days.
Can walking dislodge a DVT?
The authors concluded that walking exercise was safe in acute deep venous thrombosis (DVT) and may improve acute symptoms. Exercise training did not acutely increase leg symptoms of previous DVT and may prevent or improve post-thrombotic syndrome.
Should you be on bed rest with a DVT?
Bed rest has been considered as the cornerstone of management of deep vein thrombosis (DVT) for a long time, though it is not evidence-base, and there is growing evidence favoring early ambulation.
What should you not do with a DVT?
DON'T stand or sit in one spot for a long time. DON'T wear clothing that restricts blood flow in your legs. DON'T smoke. DON'T participate in contact sports when taking blood thinners because you're at risk of bleeding from trauma.
How long does it take for DVT to dissolve?
A DVT or pulmonary embolism can take weeks or months to totally dissolve. Even a surface clot, which is a very minor issue, can take weeks to go away. If you have a DVT or pulmonary embolism, you typically get more and more relief as the clot gets smaller.
How much walking should I do with a DVT?
Your goal is to walk for 30 to 45 minutes, 5 to 7 days per week. Strength training is also an important part of maintaining your overall health. It is safe to return to your routine if you already have a strength training program.
How long does it take for DVT to become PE?
Many patients worry that being physically active might cause a DVT to break off and become a PE. The risk of clot breaking off and forming a PE is mostly present in the first few days, up to ≈4 weeks, while the clot is still fresh, fragile, and not scarred.
How long does it take for leg swelling to go down after DVT?
Sometimes it takes 3-6 months for your blood clot symptoms to get better. Anytime you have new problems with your leg, you should see your health care provider. In most cases of PTS, leg pain and swelling will get better when you rest or elevate your leg.
What is the procedure to remove a clot in a patient with DVT?
In rare cases, a surgical procedure to remove the clot may be necessary. Thrombectomy involves removal of the clot in a patient with DVT. Embolectomy involves removal of the blockage in the lungs caused by the clot in a patient with PE.
What are the symptoms of DVT?
There are other conditions with signs and symptoms similar to those of DVT and PE. For example, muscle injury, cellulitis (a bacterial skin infection), and inflammation (swelling) of veins that are just under the skin can mimic the signs and symptoms of DVT. It is important to know that heart attack and pneumonia can have signs ...
What is a DVT test?
DVT. Duplex ultrasonography is an imaging test that uses sound waves to look at the flow of blood in the veins. It can detect blockages or blood clots in the deep veins. It is the standard imaging test to diagnose DVT. A D-dimer blood test measures a substance in the blood that is released when a clot breaks up.
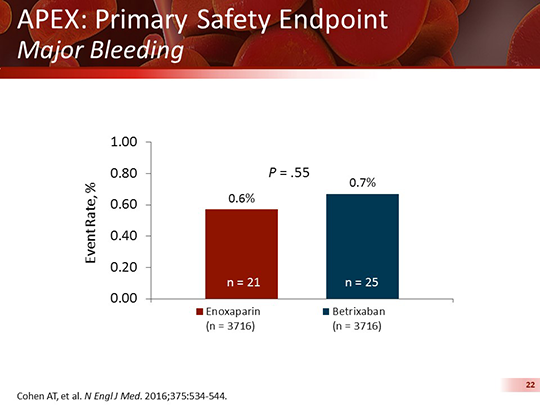
What anticoagulants are used to prevent bleeding?
Fondaparinux (injected under the skin). Anticoagulants that are taken orally (swallowed) include. Warfarin, Dabigatran, Rivaroxaban, Apixaban, and. Edoxaban. All of the anticoagulants can cause bleeding, so people taking them have to be monitored to prevent unusual bleeding.
What is CTPA in pulmonary angiography?
Computed tomographic pulmonary angiography (CTPA) is a special type of X-ray test that includes injection of contrast material (dye) into a vein. This test can provide images of the blood vessels in the lungs. It is the standard imaging test to diagnose PE.
How do thrombolytics work?
Thrombolytics (commonly referred to as “clot busters”) work by dissolving the clot. They have a higher risk of causing bleeding compared to the anticoagulants, so they are reserved for severe cases.
Can heart attack be a PE?
It is important to know that heart attack and pneumonia can have signs and symptoms similar to those of PE. Therefore, special tests that can look for clots in the veins or in the lungs (imaging tests) are needed to diagnose DVT or PE.
Is walking safe for deep vein thrombosis?
Physical activity in patients with deep venous thrombosis: a systematic review. Early walking exercise is safe in patients with acute DVT and may help to reduce acute symptoms. Exercise training does not increase leg symptoms acutely in patients with a previous DVT and may help to prevent or improve the postthrombotic syndrome.
Is it safe to walk with a DVT?
Early walking exercise is safe in patients with acute DVT and may help to reduce acute symptoms. Exercise training does not increase leg symptoms acutely in patients with a previous DVT and may help to prevent or improve the postthrombotic syndrome.
What to do if you have DVT?
If you experience DVT, your physical therapist may recommend compression therapy to improve your circulation. This involves wearing compression stockings that encourage circulation in your veins.
How to recover from DVT?
Return to Vigorous Exercise. Before engaging in moderate to vigorous exercise following a DVT diagnosis, your physical therapist should evaluate and advise you based on your individual recovery. Some therapists may be concerned that vigorous activity could cause a blood clot to dislodge and block the lung or heart.
What to do if you have a DVT after hip surgery?
If you are undergoing physical therapy after knee or hip surgery and are concerned about your risk for DVT, notify your physical therapist who can perform tests like the clinical decision rule test for the likelihood of developing DVT.
How to get rid of a blood clot in your leg?
Following an operation to remove a blood clot in the leg, your physician may recommend physical therapy to improve movement following surgery. Your therapist may engage in exercises that include improving range of motion, helping you walk with proper form and engaging in muscle strengthening exercises.
What to do if you have a blood clot?
If you have been diagnosed with condition or even required surgery to remove a blood clot, your physician may recommend physical therapy to improve circulation in your deep veins and prevent another episode.
What is the cause of deep vein thrombosis?
Deep vein thrombosis occurs when a blood clot develops in the deep veins of your upper and lower legs, an occurrence that can have deadly effects. Those who are immobile for some time, such as after bed rest or failing to move after surgery, are more likely to experience DVT. If you have been diagnosed with condition or even required surgery ...
How to move a leg after a blood clot?
Following an operation to remove a blood clot in the leg, your physician may recommend physical therapy to improve movement following surgery. A physical therapist may visit you in the hospital to help you start to move the leg in your hospital bed, such as through ankle pumps that help to encourage circulation.
How to treat DVT?
DVT is most commonly treated with anticoagulants, also called blood thinners. These drugs don't break up existing blood clots, but they can prevent clots from getting bigger and reduce your risk of developing more clots. Blood thinners may be taken by mouth or given by IV or an injection under the skin.
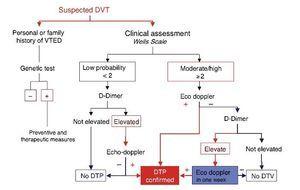
How to diagnose DVT?
Diagnosis. To diagnose DVT, your doctor will ask you about your symptoms. You'll also have a physical exam so that your doctor can check for areas of swelling, tenderness or changes in skin color. The tests you have depend on whether your doctor thinks you are at a low or a high risk of DVT. Tests used to diagnose or rule out a blood clot include: ...
What blood thinners are used for DVT?
The most commonly used injectable blood thinners for DVT are enoxaparin (Lovenox) and fondaparinux (Arixtra). After taking an injectable blood thinner for a few days, your doctor may switch you to a pill. Examples of blood thinners that you swallow include warfarin (Jantoven) and dabigatran (Pradaxa).
What blood test is used to diagnose a blood clot?
Tests used to diagnose or rule out a blood clot include: D-dimer blood test. D dimer is a type of protein produced by blood clots. Almost all people with severe DVT have increased blood levels of D dimer. A normal result on a D-dimer test often can help rule out PE. Duplex ultrasound.
How to prevent blood clots in legs?
If you've been on bed rest because of surgery or other factors, the sooner you get moving, the lower the chance that blood clots will develop. Wear compression stockings . Wear these to help prevent blood clots in the legs if your doctor recommends them.
What to do if you can't take medicine to thin your blood?
If you can't take medicines to thin your blood, you might have a filter inserted into a large vein — the vena cava — in your abdomen. A vena cava filter prevents clots that break loose from lodging in your lungs. Compression stockings. These special knee socks reduce the chances that your blood will pool and clot.
What is the procedure to check for clots in the foot?
The test is invasive, so it's rarely performed. Other tests, such as ultrasound, often are done first. Magnetic resonance imaging (MRI) scan.
What is the treatment for DVT?
Medical Management. Treatment of DVT aims to prevent pulmonary embolism, reduce morbidity, and prevent or minimize the risk of developing post-thrombotic syndrome. The cornerstone of treatment is anticoagulation. NICE guidelines only recommend treating proximal DVT (not distal) and those with pulmonary emboli.
What is the best way to prevent DVT?
A combination of mechanical and pharmacological measures can be used to prevent DVT. Mechanical prophylaxis involves the use of graduated compression stockings (GCS), intermittent pneumatic compression (IPC) and venous foot pumps to improve blood flow in the deep veins of the leg.
What are the risk factors for deep vein thrombosis?
Following are the risk factors and are considered as causes of deep venous thrombosis: Increased venous pressure: Mechanical compression or functional impairment leading to reduced flow in the veins ( neoplasm, pregnancy, varicose veins, or congenital anomaly which increases outflow resistance)
Where does DVT occur?
A deep-vein thrombosis (DVT) is a blood clot that forms within the deep veins, usually of the leg, but can occur in the veins of the arms and the mesenteric and cerebral veins.
What is the third most common cause of death from cardiovascular disease after heart attacks and stroke?
A common and important disease. It is part of the venous thromboembolism disorders which represent the third most common cause of death from cardiovascular disease after heart attacks and stroke. Account for most cases of pulmonary embolism. Only through early diagnosis and treatment can the morbidity be reduced.
What are the preventive measures for LE DVT?
For individuals who are at risk for LE DVT, preventive measures should be initiated immediately, including education regarding leg exercises, ambulation, proper hydration, mechanical compression, and assessment regarding the need for medication referral.
When should a physical therapist mobilize patients after IVC filter placement?
Physical therapists should mobilize patients after IVC filter placement once they are hemodynamically stable and there is no bleeding at the puncture site. (Evidence Quality: V; Recommendation Strength: P–Best Practice)
What is a VTE?
Venous thromboembolism (VTE) is the formation of a blood clot in a deep vein that can lead to complications, including deep vein thrombosis (DVT), a pulmonary embolism (PE), or postthrombotic syndrome (PT S). Venous thromboembolism is a serious condition, with an incidence of 10% to 30% of people dying within 1 month of diagnosis, and half of those diagnosed with a DVT have long-term complications. 1 Even with a standard course of anticoagulant therapy, one third of individuals will experience another VTE within 10 years. 1 For those who survive a VTE, quality of life can be decreased due to the need for long-term anticoagulation to prevent another VTE. 2
How do anticoagulants work?
Although anticoagulants are often referred to as blood thinners, they do not actually thin the blood. This class of drugs works by altering certain chemicals in the blood necessary for clotting to occur. Consequently, blood clots are less likely to form in the veins or arteries, and yet continue to form where needed. Although anticoagulants do not break down clots that have already formed, they do allow the body's natural clot lysis mechanisms to work normally to break down clots that have formed.
What is a physical therapist exam?
The Guide to Physical Therapist Practice states that the physical therapist examination is a comprehensive screening and specific testing process leading to diagnostic classification or, as appropriate, to a referral to another practitioner. 30 Understanding the factors that place individuals at risk for a VTE is important for all physical therapists. During the patient interview, physical therapists should ask questions and review the medical history to determine whether the patient is at risk for LE DVT. Risk factors include previous venous thrombosis or embolism, age, active cancer or cancer treatment, severe infection, oral contraceptives, hormonal replacement therapy, pregnancy or given birth within the previous 6 weeks, immobility (bed rest, flight travel, fractures), surgery, anesthesia, critical care admission, central venous catheters, inherited thrombophilia, and obesity. The relationship between particular risk factors and presence of LE DVT has been found through retrospective and prospective studies and identified as having support from level I evidence in other CPGs. 19, 31 – 34
What is a venous thromboembolism?
Venous thromboembolism is a life-threatening disorder that ranks as the third most common cardiovascular illness, after acute coronary syndrome and stroke. 4 This disorder consists of DVT and PE, 2 interrelated primary conditions caused by venous blood clots, along with several secondary conditions including PTS and CTEPH. 5 From primary and secondary prevention perspectives, the seriousness of VTE development related to mortality, morbidity, and diminished life quality is a worldwide concern. 6 The incidence of VTE differs greatly among countries. For example, the United States ranges from 70 to 120 cases per 100,000 inhabitants per year, and in Europe there are between 140 and 240 cases per 100,000 inhabitants per year, with sudden death being a frequent outcome. 7
Is reduced mobility a risk factor for VTE?
Reduced mobility is a known risk factor for VTE, yet the quantity and duration of the reduced mobility that defines degree of risk for VTE are not known. 19 – 21 Significant variability exists in the literature regarding reduced mobility and the resulting risk for VTE. 22 Patients who were ambulatory were found to be at increased risk for developing a VTE with a standing time of 6 or more hours (odds ratio [OR]=1.9) or resting in bed or a chair (OR=5.6). 23 Likewise, a significant correlation exists between loss of mobility status for 3 or more days and the presence of LE DVT on duplex ultrasound. 24
What is the risk of DVT?
Deep venous thrombosis (DVT) is a common problem among hospitalized patients, 1 even those who receive prophylaxis. 2 Patients undergoing total hip replacement have a 54% risk of developing DVT following the procedure if no methods of prophylaxis are used. 2 Use of low-molecular-weight heparin prophylaxis reduces this incidence to 16%. Despite prophylaxis, 31% of patients undergoing total knee replacement develop DVT, and 27% of patients operated on for hip fracture develop DVT. 2 Thromboembolic complications have been reported in 30% to 60% of patients following stroke. 3 Deep venous thrombosis places the patient at risk for pulmonary embolism (PE), recurrent thrombosis, and post-phlebitic syndrome. 1, 4 Up to 50% of patients with DVT involving the proximal deep veins of the lower extremity develop PE. Because the mortality rate for this condition is as high as 8% even with intervention, PE poses the greatest concern to the physical therapist and physician caring for the patient during initial management of the DVT, particularly in the hospital setting. 3
Why were patients referred to the outpatient department?
The majority of the patients included in the study were referred to the author's outpatient department because of self-reported leg symptoms. Patients with pulmonary symptoms, symptoms that indicated vascular danger to their limbs, and patients who had been immobile for the previous 2 days were excluded.
When a patient has a recentlydiagnosed LE DVT, the physical ther-apist should
When a patient has a recentlydiagnosed LE DVT, the physical ther-apist should verify whether thepatient is taking an anticoagulantmedication, what type of anticoagu-lant medication, and when theanticoagulant medication wasinitiated. (Evidence Quality: V;Recommendation Strength: D–Theoretical/Foundational)
What is venous thromboembolism?
Venous thromboembolism is a life-threatening disorder that ranks as thethird most common cardiovascular ill-ness, after acute coronary syndrome andstroke.4This disorder consists of DVTand PE, 2 interrelated primary conditionscaused by venous blood clots, along withseveral secondary conditions includingPTS and CTEPH.5From primary and sec-ondary prevention perspectives, the seri-ousness of VTE development related tomortality, morbidity, and diminished lifequality is a worldwide concern.6 Theincidence of VTE differs greatly amongcountries. For example, the United Statesranges from 70 to 120 cases per 100,000inhabitants per year, and in Europe thereare between 140 and 240 cases per100,000 inhabitants per year, with sud-den death being a frequent outcome.7
What is a VTE?
thromboembolism (VTE) isthe formation of a blood clot in adeep vein that can lead to compli-cations, including deep vein thrombosis(DVT), a pulmonary embolism (PE), orpostthrombotic syndrome (PTS). Venousthromboembolism is a serious condition,with an incidence of 10% to 30% of peo-ple dying within 1 month of diagnosis,and half of those diagnosed with a DVThave long-term complications.1 Evenwith a standard course of anticoagulanttherapy, one third of individuals willexperience another VTE within 10years.1 For those who survive a VTE,quality of life can be decreased due tothe need for long-term anticoagulation toprevent another VTE.2
How do anticoagulants work?
Although anti-coagulants are often referred to as bloodthinners, they do not actually thin theblood. This class of drugs works by alter-ing certain chemicals in the blood nec-essary for clotting to occur. Conse-quently, blood clots are less likely toform in the veins or arteries, and yetcontinue to form where needed.Although anticoagulants do not breakdown clots that have already formed,they do allow the body’s natural clot lysismechanisms to work normally to breakdown clots that have formed.
Can a LE DVT cause PE?
patient with an LE DVT is that the clotwill dislodge and embolize to the lungs,causing a potentially fatal PE. However,early ambulation has been shown to leadto no greater risk of PE than bed rest forpeople with a diagnosed LE DVT whohave been treated with anticoagulants.28
What does AAT stand for in medical terms?
Activity as Tolerated (AAT): An order given by the physician indicating that the person can be active on the ward as tolerated by the person.
How long does heparin last?
Heparin can be injected intravenously or subcutaneously (it degrades when taken by mouth) and has a half life of 1-2 hours.
Is bed rest recommended after DVT?
In the past, there have been recommendations of strict bed rest for a variable time after acute DVT and after the start of anticoagulation. More recently, research has shown that there is no difference between ambulation and bed rest on either the development of a (Pulmonary Embolism) PE (2, 8, and 9) or on the progression or development of a new DVT (5). Furthermore, the complications and cost of prescribed bed rest are well documented and early ambulation in preference to initial bed rest has been strongly recommended (9).

Diagnosis
Treatment
- There are three main goals to DVTtreatment. 1. Prevent the clot from getting bigger. 2. Prevent the clot from breaking loose and traveling to the lungs. 3. Reduce the chances of another DVT. DVTtreatment options include: 1. Blood thinners. These medicines, also called anticoagulants, help prevent blood clots from getting bigger. Blood thinners redu...
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- After DVTtreatment, follow these tips to manage the condition and prevent complications or more blood clots: 1. Ask about your diet.Foods high in vitamin K, such as spinach, kale, other leafy greens and Brussels sprouts, can interfere with the blood thinner warfarin. 2. Take medications as directed.Your provider will tell you how long you need treatment. If you're taking certain blood thi…
Preparing For Your Appointment
- DVTis considered a medical emergency. It's important to get treated quickly. If there's time before your appointment, here's some information to help you get ready.