Conventional treatment and control of ICP elevations includes general and physiologic management (cerebrospinal fluid removal, fluid restriction, controlled hyperventilation, sedation, and elevating the patient's head) and pharmacologic management.
Full Answer
What relieves rapidly increasing intracranial pressure?
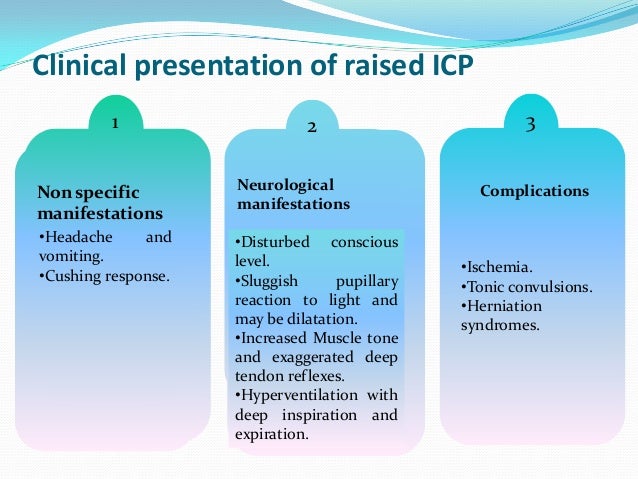
The signs of increased ICP include:
- headache
- nausea
- vomiting
- increased blood pressure
- decreased mental abilities
- confusion about time, and then location and people as the pressure worsens
- double vision
- pupils that don’t respond to changes in light
- shallow breathing
- seizures
How to manage elevated intracranial pressure?
- Maintain ICP at less than 20 to 25 mm Hg.
- Maintain CPP at greater than 60 mm Hg by maintaining adequate MAP.
- Avoid factors that aggravate or precipitate elevated ICP.
What drugs reduce intracranial pressure?
Osmotic diuretics, (e.g., urea, mannitol, glycerol) and loop diuretics (e.g., furosemide, ethacrynic acid) are first-line pharmacologic agents used to lower elevated ICP. Corticosteroids may be beneficial in some patients. Patients with elevated ICP refractory to conventional treatment may benefit from therapy with high-dose barbiturates.
How do you relieve intracranial pressure?
Global Intracranial Pressure (ICP) Monitors market influence different factors such as commercialization, development in business and revenue, and globalization to boost exhaustive growth in Intracranial Pressure (ICP) Monitors industry.
How would you treat a patient with increased intracranial pressure?
Nursing Interventions Interventions to lower or stabilize ICP include elevating the head of the bed to thirty degrees, keeping the neck in a neutral position, maintaining a normal body temperature, and preventing volume overload. The patient must be stabilized before transport to radiology for brain imaging.
What is the most appropriate management for the raised intracranial pressure?
When intracranial pressure becomes elevated, it is important to rule out new mass lesions that should be surgically evacuated. Medical management of increased intracranial pressure should include sedation, drainage of cerebrospinal fluid, and osmotherapy with either mannitol or hypertonic saline.
What medication do you give for increased ICP?
Osmotic diuretics, (e.g., urea, mannitol, glycerol) and loop diuretics (e.g., furosemide, ethacrynic acid) are first-line pharmacologic agents used to lower elevated ICP. Corticosteroids may be beneficial in some patients.
What medication is most commonly used to decrease intracranial pressure?
Osmotic diuretics, such as mannitol, may be used to decrease intracranial pressure.
Why is LP contraindicated in raised ICP?
While some patients with CT evidence of increased ICP have undergone LP without herniation, CT findings of increased ICP place patients at a dramatically increased risk for herniation if an LP is performed. Therefore, LP should be avoided when any signs of increased ICP are seen on CT.
How is ICP calculated?
0:463:56How to Calculate Cerebral Perfusion Pressure Nursing (CPP) - YouTubeYouTubeStart of suggested clipEnd of suggested clipSo I would commit this to memory it says cerebral perfusion pressure is equal to the map which isMoreSo I would commit this to memory it says cerebral perfusion pressure is equal to the map which is the mean arterial. Pressure minus the ICP which is the intracranial.
Does Lasix decrease ICP?
Abstract. Background: Mannitol and furosemide are used to reduce increased intracranial pressure (ICP) and to reduce brain bulk during neurosurgery. One mechanism by which these changes might occur is via a reduction in brain water content.
Which drug can be used to decrease intracranial or intraocular pressure?
Abstract. Purpose: Acetazolamide (ACZ) lowers intraocular pressure (IOP), acutely in normal eyes and both acutely and chronically in eyes with glaucoma, and cerebrospinal fluid pressure (CSFp), chronically in patients with idiopathic intracranial hypertension (IIH).
What does Cushing's triad indicate?
Cushing's triad refers to a set of signs that are indicative of increased intracranial pressure (ICP), or increased pressure in the brain. Cushing's triad consists of bradycardia (also known as a low heart rate), irregular respirations, and a widened pulse pressure.
What is the gold standard for measuring intracranial pressure ICP?
In terms of accuracy and reliability, the intraventricular catheter systems still remain the gold standard modality. Recent advances have led to the development of non-invasive techniques to monitor ICP, but further evidence is needed before it becomes an alternative to invasive techniques.
What causes increased intracranial pressure?
The causes of increased intracranial pressure (ICP) can be divided based on the intracerebral components causing elevated pressures: Increase in brain volume. Generalized swelling of the brain or cerebral edema from a variety of causes such as trauma, ischemia, hyperam monemia, uremic encephalopathy, and hyponatremia.
What is intracranial hypertension?
Intracranial hypertension (IH) is a clinical condition that is associated with an elevation of the pressures within the cranium. The pressure in the cranial vault is measured in millimeters of mercury (mm Hg) and is normally less than 20 mm Hg.
What should be included in an ICP evaluation?
The evaluation of increased ICP should include detailed history taking, physical examination, and ancillary studies.
What is the Cushing Triad?
Cushing triad is a clinical syndrome consisting of hypertension, bradycardia and irregular respiration and is a sign of impending brain herniation. This occurs when the ICP is too high the elevation of blood pressure is a reflex mechanism to maintain CPP.
How to measure ICP?
The use of ultrasound to measure the diameter of the optic nerve sheath has been recently identified as a method to indicate raised ICP. This is usually measured 3 mm behind the globe with 2–3 measurements taken in each eye. The threshold for denoting elevated ICP usually ranges from 0.48 cm to 0.63 cm.
What is the pressure in the cranial vault?
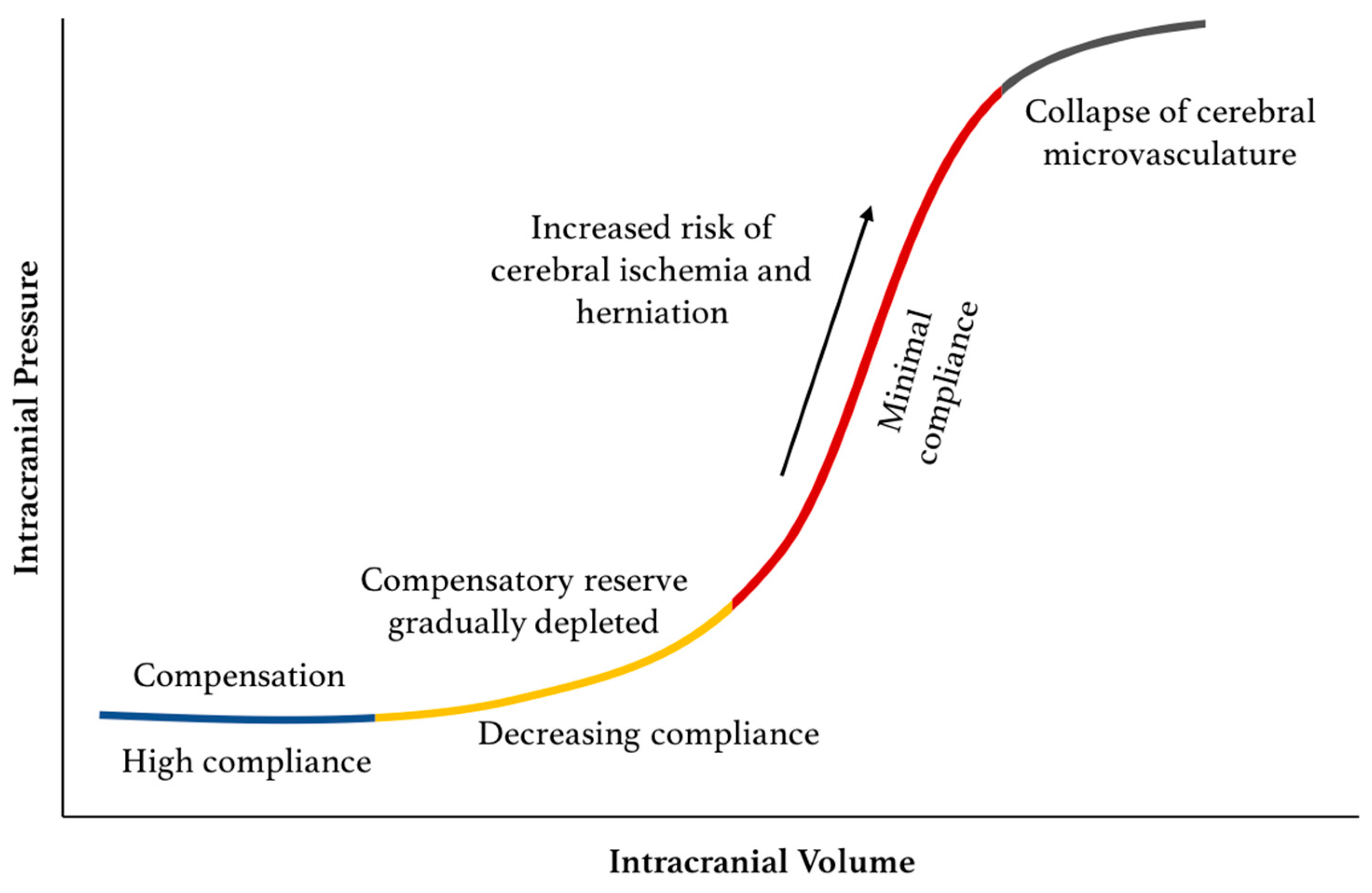
The pressure in the cranial vault is measured in millimeters of mercury (mm Hg) and is normally less than 20 mm Hg. The cranium is a rigid structure that contains three main components: brain, cerebrospinal fluid, and blood. Any increase in the volume of its contents will increase the pressure within the cranial vault.
What is the cranial vault?
The cranium is a rigid structure that contains 3 main components: brain, cerebrospinal fluid, and blood. Any increase in the volume of its contents will increase the pressure within the cranial vault. An increase in the volume of one component will result in a decrease of volume in 1 or 2 of the other components.
What is intracranial pressure?
Summary. Increased intracranial pressure is a medical term that refers to growing pressure inside a person’s skull. This pressure can affect the brain if doctors do not treat it. A sudden increase in the pressure inside a person’s skull is a medical emergency.
What to do if ICP is increased?
If a person has a diagnosis of increased ICP, a doctor will immediately work to reduce the pressure inside the skull to lessen the risk of brain damage. They will then work to treat the underlying cause of the increased pressure.
Why is ICP high in infants?
In infants, high ICP may be the result of child abuse. If a person handles a baby or infant too roughly, it may cause them to develop a brain injury. This is known as shaken baby syndrome. One source has estimated that between 1,000 and 3,000 children in the United States experience shaken baby syndrome each year.
What are the symptoms of increased ICP?
Symptoms of increased ICP in adults include: pupils that do not respond to light in the usual way. headache. behavior changes. reduced alertness. sleepiness. muscle weakness. speech or movement difficulties. vomiting.
What is the normal range for ICP?
A doctor will measure the ICP in millimeters of mercury (mm/Hg). The normal range is less than 20 mm/Hg. Trusted Source.
How to diagnose increased ICP?
a previous diagnosis of a brain tumor. Then, the doctor may carry out the following tests: neurological exam to test a person’s senses, balance, and mental state. spinal tap that measures cerebrospinal fluid pressure.
Why drain cerebrospinal fluid?
draining the excess cerebrospinal fluid with a shunt, to reduce pressure on the brain that hydrocephalus has caused
What is the best treatment for intracranial hypertension?
Medical management of increased intracranial pressure should include sedation, drainage of cerebrospinal fluid, and osmotherapy with either mannitol or hypertonic saline. For intracranial hypertension refractory to initial medical management, barbiturate coma, hypothermia, or decompressive craniectomy should be considered. Steroids are not indicated and may be harmful in the treatment of intracranial hypertension resulting from traumatic brain injury.
What is intracranial hypertension?
Intracranial hypertension is an important cause of secondary injury in patients with acute neurologic and neurosurgical disorders and typically mandates specific monitoring. Patients with suspected intracranial hypertension, especially secondary to TBI, should have monitoring of ICP; monitoring of cerebral oxygen extraction, as with jugular bulb oximetry or brain tissue PO2, may also be indicated. Brain-injured patients also should have close monitoring of systemic parameters, including ventilation, oxygenation, electrocardiogram, heart rate, blood pressure, temperature, blood glucose, and fluid intake and output. Patients should be monitored routinely with pulse oximetry and capnography to avoid unrecognized hypoxemia and hypoventilation or hyperventilation. A central venous catheter commonly is needed to help evaluate volume status, and a Foley catheter is employed for accurate urine output.
What is the normal ICP for a child?
The normal range for ICP varies with age. Values for pediatric subjects are not as well established. Normal values are less than 10 to 15 mm Hg for adults and older children, 3 to 7 mm Hg for young children, and 1.5 to 6 mm Hg for term infants. ICP can be subatmospheric in newborns [4]. For the purpose of this article, normal adult ICP is defined as 5 to 15 mm Hg (7.5–20 cm H2O). ICP values of 20 to 30 mm Hg represent mild intracranial hypertension; however, when a temporal mass lesion is present, herniation can occur with ICP values less than 20 mm Hg [5]. ICP values greater than 20 to 25 mm Hg require treatment in most circumstances. Sustained ICP values of greater than 40 mm Hg indicate severe, life-threatening intracranial hypertension.
What is the best device for monitoring ICP?
The ventriculostomy catheter is the preferred device for monitoring ICP and the standard against which all newer monitors are compared [20]. An intraventricular catheter is connected to an external pressure transducer via fluid-filled tubing. The advantages of the ventriculostomy are its relatively low cost, the option to use it for therapeutic CSF drainage, and its ability to recalibrate to minimize errors owing to measurement drift. The disadvantages are difficulties with insertion into compressed or displaced ventricles, inaccuracies of the pressure measurements because of obstruction of the fluid column, and the need to maintain the transducer at a fixed reference point relative to the patient’s head. The system should be checked for proper functioning at least every 2 to 4 hours, and any time there is a change in the ICP, neurologic examination, and CSF output. This check should include assessing for the presence of an adequate waveform, which should have respiratory variations and transmitted pulse pressure.
How does CPP affect ICP?
When CPP is within the normal autoregulatory range (50–150 mmHg), this ability of the brain to pressure autoregulate also affects the response of ICP to a change in CPP [6–8]. When pressure autoregulation is intact, decreasing CPP results in vasodilation of cerebral vessels, which allows CBF to remain unchanged. This vasodilation can result in an increase in ICP, which further perpetuates the decrease in CPP. This response has been called the vasodilatory cascade. Likewise, an increase in CPP results in vasoconstriction of cerebral vessels and may reduce ICP. When pressure autoregulation is impaired or absent, ICP decreases and increases with changes in CPP.
How long does it take for ICP to increase after trauma?
A secondary increase in the ICP often is observed 3 to 10 days after the trauma, principally as a result of a delayed hematoma formation, such as epidural hematomas, acute subdural hematoma, and traumatic hemorrhagic contusions with surrounding edema, sometimes requiring evacuation [16]. Other potential causes of delayed increases in ICP are cerebral vasospasm [17], hypoventilation, and hyponatremia.
What is the cranial fontanelle?
In normal individuals with closed cranial fontanelles, central nervous system contents, including brain, spinal cord, blood, and cerebrospinal fluid (CSF), are encased in a noncompliant skull and vertebral canal, constituting a nearly incompressible system. There is a small amount of capacitance in the system provided by the intervertebral spaces. In the average adult, the skull encloses a total volume of 1450 mL: 1300 mL of brain, 65 mL of CSF, and 110 mL of blood [1]. The Monroe-Kellie hypothesis states the sum of the intracranial volumes of blood, brain, CSF, and other components is constant, and that an increase in any one of these must be offset by an equal decrease in another, or else pressure increases. An increase in pressure caused by an expanding intracranial volume is distributed evenly throughout the intracranial cavity [2,3].
What is increased intracranial pressure?
Description. Increased intracranial pressure is a rise in the pressure inside the skull that can result from or cause brain injury. is the pressure in the skull that results from the volume of three essential components: cerebrospinal fluid (CSF), intracranial blood volume and central nervous system tissue. The normal intracranial pressure is ...
How to treat increased ICP?
A drastic treatment for increased ICP is decompressive craniectomy, in which a part of the skull is removed and the dura mater is expanded to allow the brain to swell without crushing it or causing herniation.The section of bone removed, known as a bone flap, can be stored in the patient’s abdomen and recited back to complete the skull once the acute cause of raised ICP’s has resolved. Alternatively a synthetic material may be used to replace the removed bone section.
How does mannitol help with diuresis?
Mannitol promotes osmotic diuresis by increasing the pressure gradient, drawing fluid from intracellular to intravascular spaces. Although mannitol is used for all the reasons described, the reduction of ICP in this client is a concern.
How high should the head of the bed be when a client has increased intracranial pressure?
The nurse should avoid flexing or extending the client’s neck or turning the head side to side. The head of the bed should be raised to 30 to 45 degrees.
Why do they do craniotomy?
Craniotomies are holes drilled in the skull to remove intracranial hematomas or relieve pressure from parts of the brain.As raised ICP’s may be caused by the presence of a mass, removal of this via craniotomy will decrease raised ICP’s.
What are the signs of ICP?
In general, symptoms and signs that suggest a rise in ICP including headache, vomiting without nausea, ocular palsies, altered level of consciousness, back pain and papilledema. If papilledema is protracted, it may lead to visual disturbances, optic atrophy, and eventually blindness.
How much blood is in the cranial vault?
The intact cranium is essentially inexpandable containing about 1400 grams of central nervous system (CNS) or brain tissue, 75 ml of blood and about 75 ml of cerebrospinal fluid (CSF). These three components of the cranial vault maintain a state of equilibrium.
What is elevated intracranial pressure?
Elevated intracranial pressure (ICP), is a build-up of pressure in the skull. Whether it's caused by swelling, bleeding, a tumor, or some other problem, ICP can lead to compression of brain tissue and cause permanent damage. That's why it's considered a neurological emergency that needs to be addressed as soon as possible.
What to do if brain is squeezed?
If the brain is being squeezed by something in the skull that doesn’t belong there, like an abscess or tumor, removing it can be the answer. Another tactic is to insert a shunt in the brain through which excess CSF can drain.
How to tell if someone is unconscious with ICP?
To tell if a person who's unconscious is experiencing ICP, a doctor or other medical professional usually will rely on fundoscopy , which involves lifting up an eyelid and using a bright light to illuminate the back ...
Why is it important to measure ICP?
This is especially useful when it's likely ICP will get worse , such as after brain trauma that causes swelling.
How to measure ICP?
To measure the increase in pressure, a monitor can be placed beneath the skull. This has the added benefit of being able to measure ICP constantly rather than just getting a single measurement, so changes in ICP can be captured. This is especially useful when it's likely ICP will get worse, such as after brain trauma that causes swelling.
How to make the brain bigger?
Another approach is to make the brain space bigger. This is done in a procedure called a craniectomy, in which a portion of the skull is removed temporarily so the brain has room to swell. It sounds scary, and it is a very risky thing to do, but when swelling is so severe that a craniectomy is necessary there really are no other options. 4 During the period of time when the skull is removed, the tissue surrounding the brain is kept intact and clean as possible to prevent infection.
What happens when you intubate a patient?
If a patient is intubated (has a breathing tube in), the breathing rate can be increased to change the acidity of the patient’s blood, which will cause the arteries in the brain to narrow, reduce blood flow, and clear more room for the brain —a temporary solution at best.
What causes increased ICP?
Increased ICP is defined by an increase in pressure in the skull caused by an increase in the volume of brain tissue, blood, cerebrospinal fluid, or by the presence of a space occupying lesion. The increased pressure compresses brain tissue, which causes damage to the neurons leading to neuron changes, eventual herniation and brain death.
What causes increased pressure in the cranial cavity?
Increased pressure within the cranial cavity (or skull) is caused by an increase in the volume of either the brain tissue, blood, or cerebrospinal fluid, or by the presence of another space-occupying lesion. This increased pressure will compress the brain tissue, causing damage to the neurons and leading to neuro changes ...
What causes increased volume of brain tissue, blood, or cerebrospinal fluid within the skull?
Anything that causes increased volume of brain tissue, blood, or cerebrospinal fluid within the skull – cerebral edema, hemorrhage, hydrocephalus, hypertension, cerebral vasodilation. Could also be caused by a space-occupying lesion such as a tumor or mass.
Why do they do a craniectomy?
A craniectomy is used to remove a portion of the skull (bone flap) in order to allow space for cerebral swelling.
What is the temperature of a patient with a loss of autonomic regulation?
With a loss of autonomic regulation, a patient’s temperature could become very elevated (104°+).
Can ICP be increased by 30?
Below 30 and above 45 can both increase ICP. You also want to decrease stimuli as agitation can increase ICP in your patient, and avoid Valsalva maneuvers because coughing and bearing down can increase ICP also. Here is a look at the completed care plan for increased ICP. Let’s do a quick review.
What is elevated ICP?
Elevated ICP can be associated with severe head injuries and diseases of the central nervous system such as brain tumors and stroke. Symptoms of elevated ICP may be difficult to distinguish from symptoms of other disease states.
Can corticosteroids be used for elevated ICP?
Corticosteroids may be beneficial in some patients. Patients with elevated ICP refractory to conventional treatment may benefit from therapy with high-dose barbiturates. Pentobarbital has been used in the majority of the clinical studies.
What is intracranial hypertension?
Intracranial hypertension (IH) is a common clinical problem in the intensive care unit (ICU), which requires immediate and urgent treatment . IH is the result of either primary central nervous system (CNS) lesion or a complication of co-existing systemic disease. It is caused by a variety of conditions divided into five main categories based on their pathological mechanism (Table (Table1).1). Any condition affecting the CNS, defined as acute brain injury (ABI) [(e.g. traumatic brain injury (TBI)], has two components: primary brain injury that cannot be reversed and secondary brain injury (SBI). SBI is defined as any physiological event that can occur within minutes, hours, or days after the initial injury and leads to further damage of nervous tissue. It can be detected through clinical examination and intracranial pressure (ICP) monitoring, as it is mostly due to increased ICP, and confirmed by imaging tests. Since there is a causal relationship between primary brain injury, IH, and SBI (Fig. 1), we focus on IH in this article. We conducted a literature search on MEDLINE/PubMed and Cochrane Library for studies completed in the last twenty years using the terms "intracranial hypertension" and "ICU management". We have also included guidelines from all established societies regarding IH in ABI [TBI, intracerebral hemorrhage (ICH), aneurysmal subarachnoid hemorrhage (SAH), ischemic stroke] and its management in ICU. The aim of this review article is to provide basic knowledge updated with what's new in the literature regarding the management of patient with IH.
What is the purpose of ICP monitoring?
In clinical practice, invasive and non-invasive methods of ICP monitoring are used aiming to determine the optimal cerebral perfusion pressure (CPP).
What is CT evaluation?
CT evaluates rapidly the presence of specific findings that enhance the diagnosis of ΙΗ. These include mass effect, midline shift, cerebral edema, hydrocephalus, compression of basal cisterns and changes in grey-white matter differentiation.
Can MRI show diffuse axonal injury?
MRI shows in more detail soft tissu e and cerebral parenchymal les ions, which may not have been detected on CT, e.g. diffuse axonal injury. However, the prolonged screening time and stay of the patient in the supine position, which may aggravate ICP, make its use limited to patients with suspected IH.
Can cerebral edema be placed in the brain?
Difficult to place into brains with severe cerebral edema
Is IH a clinical manifestation?
The clinical manifestations of IH are nonspecific and their severity does not correlate with the degree of IH (Table (Table2).2). The comatose patient with ABI and possible IH should be clinically evaluated using routinely either the Glasgow coma scale (GCS) (combined with assessment of pupils) or the full outline of unresponsiveness (FOUR) score, as multimodality monitoring (MMM) consensus recommend [1]. Brain herniation is a potentially fatal complication of IH. There are six types of herniation, namely the uncal transtentorial, the central transtentorial, the subfalcine, the tonsilar, the ascending transtentorial and the transcalvarial herniation (Fig. 2).
Does ONSD increase ICP?
Thus, ONSD measured using a transocular ultrasound is increased in patients with IH. Several studies have shown that ONSD > 5 mm corresponds to ICP ≥ 20 mmHg [14, 15]. However, this association may be affected by conditions, such as tumors, inflammation, Grave’s disease and sarcoidosis, which may alter ONSD. The ONSD measurement technique is cheap, efficient and non-time consuming, but operator dependent [10].