
Medication
You can take steps to care for your body if you have rheumatoid arthritis. These self-care measures, when used along with your rheumatoid arthritis medications, can help you manage your signs and symptoms: Exercise regularly. Gentle exercise can help strengthen the muscles around your joints, and it can help fight fatigue you might feel.
Procedures
There is no cure for rheumatoid arthritis. But recent discoveries indicate that remission of symptoms is more likely when treatment begins early with strong medications known as disease-modifying antirheumatic drugs (DMARDs).
Therapy
The ACR updates its guideline for the treatment of rheumatoid arthritis (RA) every few years. The last changes appeared in 2015. Since then, new drugs have hit the market, older drugs have been reassessed, and there’s more evidence for the role of nondrug treatments for RA.
Self-care
There are many different rheumatoid arthritis pain management practices for patients to incorporate into their treatment. Some of the most effective and widely used rheumatoid arthritis pain management practices include: Choosing the right medications. Heat and cold packs.
Nutrition
How can I Manage my rheumatoid arthritis on a daily basis?
Is there a cure for rheumatoid arthritis?
How often does the ACR update its guidelines for rheumatoid arthritis (RA)?
What are the different rheumatoid arthritis pain management practices?
What is the most successful treatment for rheumatoid arthritis?
Methotrexate is usually the first medicine given for rheumatoid arthritis, often with another DMARD and a short course of steroids (corticosteroids) to relieve any pain. These may be combined with biological treatments.
What is the recommended treatment for rheumatoid arthritis?
Conventional DMARDs . These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include methotrexate (Trexall, Otrexup, others), leflunomide (Arava), hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine).
What is the safest treatment for rheumatoid arthritis?
Hydroxychloroquine. Hydroxychloroquine is an antimalarial drug which is relatively safe and well-tolerated agent for the treatment of rheumatoid arthritis.
Does rheumatoid arthritis always need treatment?
Treating rheumatoid arthritis There's no cure for rheumatoid arthritis. However, early diagnosis and appropriate treatment enables many people with the condition to have periods of months or even years between flares. This can help them to lead full lives and continue regular employment.
What is the number one medication for rheumatoid arthritis?
Doctors usually first prescribe methotrexate (Rheumatrex, Trexall) to treat rheumatoid arthritis. If that alone doesn't calm the inflammation, they may try or add a different type of conventional DMARD such as hydroxychloroquine (Plaquenil), leflunomide (Arava), sulfasalazine (Azulfidine), or tofacitinib (Xeljanz).
What triggers rheumatoid arthritis?
Rheumatoid arthritis is an autoimmune condition, which means it's caused by the immune system attacking healthy body tissue. However, it's not yet known what triggers this. Your immune system normally makes antibodies that attack bacteria and viruses, helping to fight infection.
Is hydroxychloroquine safer than methotrexate?
Safety variables at 6 month were within normal physiological ranges and did not differ in groups (p>0.05) indicating that both methotrexate and hydroxychloroquine were effective and safe to use in rheumatoid arthritis. The difference in the incidence of adverse effects, total or individual, was almost nil.
What is the life expectancy of a person with rheumatoid arthritis?
The average duration of disease were 10.5 years in male patients and 17.7 years in female. The average life span of the patients with RA, revealing 65.8 years in male and 63.7 years in female, were much shorter than of general population. The causes of all deaths were investigated by ourselves and/or autopsy.
How can I reverse rheumatoid arthritis naturally?
Receiving massage regularly will help you send your arthritis into remission.Exercises and physical therapy. One of the main proven treatments to reverse rheumatoid arthritis is exercises and physical therapy. ... Probiotics to Reverse Rheumatoid Arthritis. ... Other Supplements and Magnesium Oil.
Can you stop rheumatoid arthritis from progressing?
Rheumatoid arthritis (RA) is a chronic condition for which there is no cure. But even though the disease is progressive, newer disease-modifying drugs may actually be able to slow or even halt it getting worse.
Can rheumatoid arthritis go away?
Rheumatoid arthritis is a lifelong disease. When it's treated, it may go away for a little while, but it usually comes back. It's important to see your doctor as soon as symptoms begin. The earlier you start treatment, the better your outcome.
Can you manage RA without medication?
You'll need to keep up with your usual medical care, but some natural remedies might help relieve pain and stiffness from rheumatoid arthritis (RA). Many of them are simple, like using heat and ice packs. Others, like acupuncture, need a trained pro.
What is the goal of rheumatoid arthritis treatment?
The goal of rheumatoid arthritis treatment now aims toward achieving the lowest possible level of arthritis disease activity and remission if possible, minimizing joint damage, and enhancing physical function and quality of life.
What are the different types of rheumatoid arthritis drugs?
There are three general classes of drugs commonly used in the treatment of rheumatoid arthritis: non-steroidal anti-inflammatory agents (NSAIDs), corticosteroids, and disease modifying anti-rheumatic drugs (DMARDs). NSAIDs and corticosteroids have a short onset of action while DMARDs can take several weeks or months to demonstrate a clinical effect. DMARDs include methotrexate, sulfasalazine, leflunomide (Arava®), etanercept (Enbrel®), infliximab (Remicade®), adalimumab (Humira®), certolizumab pegol (Cimzia®), golimumab (Simponi®), abatacept (Orencia®), rituximab (Rituxan®), tocilizumab (Actemra®), anakinra (Kineret®), antimalarials (e.g. Plaquenil®). Other immunomodulators are occasionally used including azathioprine (Imuran) and cyclosporine. Because cartilage damage and bony erosions frequently occur within the first two years of disease, rheumatologists now move aggressively to a DMARD agent early in the course of disease, usually as soon as a diagnosis is confirmed. Analgesic drugs are also sometimes helpful in decreasing pain until DMARDs take effect. A summary table of how to monitor drug treatment in rheumatoid arthritis is included.
How long does it take for folic acid to work after methotrexate?
These side effects can often be overcome by increasing folic acid or using an activated form of folic acid known as folinic acid (leukovorin®) given as a 5mg dose 12 hours and sometimes 24 hours after methotrexate is given. Some patients complain of GI upset (nausea or diarrhea) with oral methotrexate.
How long does it take for NSAIDS to work?
Usual Time to Effect: The onset of action is seen in as early as 4 to 6 weeks.
Why is rest important for musculoskeletal health?
Because obesity stresses the musculoskeletal system , ideal body weight should be achieved and maintained. Rest, in general, is an important feature of management. When the joints are actively inflamed, vigorous activity should be avoided because of the danger of intensifying joint inflammation or causing traumatic injury to structures weakened by inflammation. On the other hand, patients should be urged to maintain a modest level of activity to prevent joint laxity and muscular atrophy. Splinting of acutely inflamed joints, particularly at night and the use of walking aids (canes, walkers) are all effective means of reducing stress on specific joints. A consultation with a physical and an occupational therapist is recommended early in the course.
Is there a cure for rheumatoid arthritis?
Rheumatoid arthritis is a chronic disorder for which there is no known cure . Fortunately in the last few years, a shift in strategy toward the earlier institution of disease modifying drugs and the availability of new classes of medications have greatly improved the outcomes that can be expected by most patients.
Is Johns Hopkins Arthritis Center educational?
All information contained within the Johns Hopkins Arthritis Center website is intended for educational purposes only. Physicians and other health care professionals are encouraged to consult other sources and confirm the information contained within this site. Consumers should never disregard medical advice or delay in seeking it because of something they may have read on this website.
How to treat RA?
Keeping an active, healthy lifestyle is just as important in treating RA symptoms as the right combination of medications. Exercise may seem too painful, but low-risk exercises like walking and yoga can reduce inflammation. A physical therapist can help you design a safe, effective daily workout routine that will keep joints flexible.
How does a physical therapist help with RA?
Physical therapists can help patients learn appropriate exercises and new ways of approaching tasks that minimize the strain on affected joints while improving overall body strength.
What is the best medication for pain?
NSAIDs, or non-steroidal anti-inflammatory drugs, are medications meant to relieve pain and reduce inflammation. They are available over-the-counter, and when needed, stronger doses may be prescribed. Many people are already familiar with NSAIDs because they are used to treat headaches, fevers and other common ailments safely at home. Ibuprofen (Advil, Motrin IB) and naproxen (Aleve) are two basic NSAIDs that will reduce pain and inflammation temporarily.
What doctor treats rheumatoid arthritis?
There are many ways to treat rheumatoid arthritis, and a doctor or rheumatologist can help determine which methods are best for each patient’s individual needs.
What is tight control for RA?
Depending on the severity of your symptoms, the goals of treatment will be to gain “tight control” of RA, meaning the disease’s activity is kept steadily at a low level. Keeping RA in “tight control” can prevent long-term joint damage. These goals primarily focus on:
When replacements aren't possible, can surgeons fuse and realign joints?
Joint fusion — when replacements aren’t possible, surgeons can fuse and realign joints
Do weaker NSAIDs slow down disease?
Weaker NSAIDs come with little side effects or risks but they also only manage symptoms and pain — they will not help with slowing disease activity.
What is the best treatment for rheumatoid arthritis?
Methotrexate. Methotrexate is a conventional disease-modifying anti-inflammatory drug (DMARD). It works to lower inflammation and slow an overactive immune system, which occurs in rheumatoid arthritis. The new guidelines strongly recommend methotrexate alone (monotherapy) as the first treatment for people with moderate to high disease activity who ...
When was the last time the ACR updated its guidelines for rheumatoid arthritis?
The ACR updates its guideline for the treatment of rheumatoid arthritis (RA) every few years. The last changes appeared in 2015. Since then, new drugs have hit the market, older drugs have been reassessed, and there’s more evidence for the role of nondrug treatments for RA.
What is the most important factor in all treatment considerations?
The most important factor in all treatment considerations is shared decision-making, where patients are informed of all their options, including nondrug ones, and have a full voice in their own care. “Patients were involved in every step of the process [of creating the update], and the recommendations truly reflect their perspectives,” Dr. Fraenkel says.
What is the treatment to target approach?
Although there’s not much evidence to support it, a treat-to-target approach is strongly recommended for patients who haven’t taken biologics or small molecule drugs. In treat-to-target, doctors and patients decide on a goal and adjust treatment until the goal is reached. Though everyone hopes for remission, many patients may not be able to achieve it. A more realistic aim is low disease activity, which keeps symptoms under control and helps maintain a good quality of life. Still, the guideline states the goal should be tailored to each patient and remission can be the target when possible.
Can you take corticosteroids as a bridge?
In an effort to greatly limit the use of corticosteroids, even as a bridge treatment, the guidelines strongly recommend against long-term steroids and conditionally recommend against short-term steroid use.
Is methotrexate monotherapy or adalimumab?
The new guidelines strongly recommend metho trexate alone (monotherapy) as the first treatment for people with moderate to high disease activity who haven’t taken DMARDs before. Methotrexate mono therapy is strongly recommended over other conventional DMARDs, a biologic DMARD like adalimumab ( Humira) and small molecule drugs such as Janus kinase ...
How to treat RA?
There are three primary strategies that doctors follow when treating RA patients with medications. These treatment strategies include: 1 Aggressively treating symptoms as early as possible 2 Targeting remission to eliminate signs of inflammation for as long as possible 3 Tightly controlling disease activity to keep it to a minimum and to prevent further joint damage
How to treat RA with medication?
These treatment strategies include: Aggressively treating symptoms as early as possible. Targeting remission to eliminate signs of inflammation for as long as possible.
How long does it take for DMARDs to work?
Some patients may find that DMARDs take up to six months to start working. One of the most commonly known DMARDs is methotrexate. There are others commonly used like leflunomide, hydroxychloroquine, and sulfasalazine, which are often prescribed to RA patients.
What is the name of the drug that is used for RA?
This form of medication is only taken by injection, unlike the others which are typically oral medications. Some of the most common brand names of RA biologics include Humira, Amjevita, Rituxan, Orencia, and many more. Biologics are a newer form of RA medication and so the long-term side effects, if any, are unknown at the present.
What is biologics in RA?
Biologics. Biologics, or biological response modifiers, are a type of DMARD. Biologics alleviate RA symptoms by targeting the part of the immune system that attacks joint tissue and causes inflammation. Biologics are also found to work effectively on moderate to severe cases of RA.
Why have RA medications evolved over time?
RA medications have greatly evolved over time as a result of the ongoing need for treating these patients and their varying symptoms.
What is the best medicine for RA?
This is crucial for allowing patients to maintain their quality of life. The two most common types of NSAIDs are ibuprofen and naproxen, which are well-known and commonly available by the brand names of Advil and Aleve, ...
How to treat RA early?
But many experts are taking a more aggressive approach, treating RA early with powerful drugs and using drug combinations rather than a single medication. There are several reasons for this. Studies have shown a link between ongoing RA inflammation and an increased rate of death and illness. Also, more effective therapeutic drugs have become available, and it has been shown that drug combinations can improve long-term outcomes. For women whose joint damage is severe and a source of constant pain, surgery may be the best option. Artificial joints and procedures to reconstruct tendons can restore function and dramatically improve quality of life.
How many classes of drugs are there for RA?
Three classes of drugs help relieve RA symptoms, although they don't influence the overall course of the disease.
What blood test is used to determine if you have rheumatoid arthritis?
The diagnostic process may involve a variety of blood tests, including erythrocyte sedimentation rate (a general measure of inflammation), a complete blood count, and a test for rheumatoid factor — an antibody found in the blood of most people who have rheumatoid arthritis.
What are the symptoms of rheumatoid arthritis?
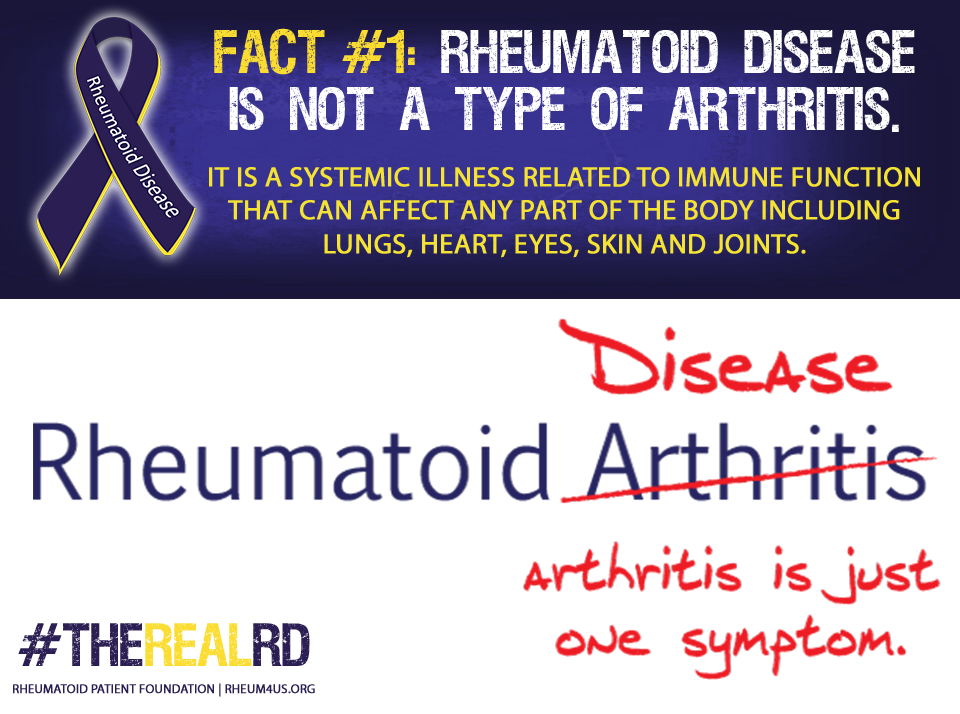
Rheumatoid arthritis can also attack tissues in addition to the joints, causing further symptoms. Fatigue and fever are common. Lymph nodes may swell. Some people develop nodules (lumps of tissue) beneath the skin near the joints, or in bony areas often exposed to pressure, such as the elbow and the forearm. In about 40% of RA cases, the pericardium — the tissue sac that encircles the heart — becomes inflamed. Inflammation may also occur in the lining of the lungs (pleuritis) or in the tear ducts and salivary glands, resulting in dry eyes and mouth. Some people develop anemia (a low red blood cell count).
What are the symptoms of arthritis in the upper part of the body?
Symptoms and causes. The affected joints feel warm, swollen, and tender. They may be stiff when you wake up and ache after you rest. Rheumatoid arthritis often strikes the wrists and the upper part of the fingers. The neck, shoulders, hips, knees, ankles, and feet may also be affected.
Why do we need x-rays for rheumatoid arthritis?
Once such damage has occurred, x-rays may be used to monitor the progression of the disease or the effects of therapy. Anatomy of rheumatoid arthritis. Joints (the places where bones meet) are surrounded by a capsule lined with a membrane called synovium.
What causes dry eyes and mouth with RA?
In about 40% of RA cases, the pericardium — the tissue sac that encircles the heart — becomes inflamed. Inflammation may also occur in the lining of the lungs (pleuritis) or in the tear ducts and salivary glands, resulting in dry eyes and mouth. Some people develop anemia (a low red blood cell count).
What is the best way to treat RA?
The best care comes from a multidisciplinary team. Your rheumatologist may refer you to a physical or occupational therapist. Many people with RA have trouble at work or home when their disease is active. These professionals can help rheumatologists figure out ways to help you thrive at work. It’s rare, but medications and the disease itself can affect other organs. Your doctor may need to refer you to other specialists. If you already have significant damage, orthopedic surgeons can help repair your joints. And it’s critical to have a primary care physician who keeps an eye on your overall health. When you have other diseases like diabetes that aren’t well controlled, it makes it harder to get your RA under control.
What is the first line of treatment for RA?
The first-line RA treatments are oral DMARDs such as, hydroxychloroquine, leflunomide, methotrexate, and sulfasalazine, sometimes used in combination with each other. We choose these first because they have great treatment and safety profiles and they’re less expensive.
How to take DMARDs?
You can take DMARDs by mouth or get them as an injection under your skin or an infusion into a vein. In the midst of the COVID-19 pandemic, it’s important to know that these medications work by suppressing your immune system, which puts you at greater risk of infection. Your rheumatologist can help you understand the risks and benefits of treatment, but data suggests that in most cases, you should still take DMARDs if you have active RA.
How long does it take for DMARDs to work?
DMARDs start working in 2 to 4 weeks, but often take longer to reach their greatest effect. You might get additional treatments, too. We also use pain medications and steroids in the short term until the DMARDs kick in.
What is the most important thing to have with a rheumatologist?
The single most important thing is to have an open and close relationship with your rheumatologist. Most rheumatologists are extremely interested in hearing what your goals for treatment are so they can tailor their recommendations to include your preferences. Even if you hate medications, your rheumatologist can talk to you about the risks and benefits of various approaches.
What is the central concept of RA?
These terms both relate to the most important central concept in RA: Inflammation = joint damage. We want to keep the symptoms under the tightest possible control (ideally no or very few symptoms) because this is a sign the inflammation is under control and the damage to your joints will be minimized.
What are some exercises to help with RA?
Any exercise that doesn’t cause pain is good. Aerobic exercise that gets your heart rate up helps with fatigue, sleep, and heart health (people with RA are at higher risk of heart attack than the average person). Light weightlifting can build muscle, which helps support bones. But don’t overdo it. The expression “no pain, no gain” doesn’t really apply here. When you have RA, pain is a sign of inflammation. You shouldn’t ignore it. Many people with RA are unable to run even moderate distances due to pressure on the joints so swimming or walking in water can be helpful because the water relieves some pressure on your joints. Walking, bicycling, light yoga, and tai chi are also good options.

Diagnosis
Treatment
Clinical Trials
Lifestyle and Home Remedies
Specialist to consult
Coping and Support
- Rheumatoid arthritis can be difficult to diagnose in its early stages because the early signs and symptoms mimic those of many other diseases. There is no one blood test or physical finding to confirm the diagnosis. During the physical exam, your doctor will check your joints for swelling, r…
Preparing For Your Appointment
- There is no cure for rheumatoid arthritis. But clinical studies indicate that remission of symptoms is more likely when treatment begins early with medications known as disease-modifying antirheumatic drugs (DMARDs).