What is allergic rhinitis and how is it treated?
Jun 18, 2019 · Definition and forms of allergic rhinitis. Allergic rhinitis (AR) is an inflammatory process of the nasal mucosa, typically IgE-mediated, elicited by environmental allergens and characterized by the presence of inflammatory cells within the mucosa and submucosa [].The course of the disease involves one or more of the symptoms enumerated below, persisting for …
Can nasal sprays help nonallergic rhinitis?
Oct 01, 2014 · A simple, safe and inexpensive treatment for allergic rhinitis consists of rinsing nasal cavities using isosaline irrigation . Nasal saline irrigation produced, according to this recent meta-analysis, a 27% improvement in nasal symptoms, a 62% reduction in medicine consumption, a 31% acceleration of mucociliary clearance time, and a 27% improvement in quality of life.
What is the prognosis of allergic rhinitis (AR)?
Jan 09, 2022 · 1. Introduction. Chronic rhinitis may be divided into two groups: allergic rhinitis (AR) and non-allergic non-infectious rhinitis, often simplified as non-AR (NAR) [1,2].Due to its increasing incidence worldwide as well as its impact on quality of life, school performance, and productivity at work, AR has become an important public health issue []. ...
What are the risks of immunotherapy for allergic rhinitis?
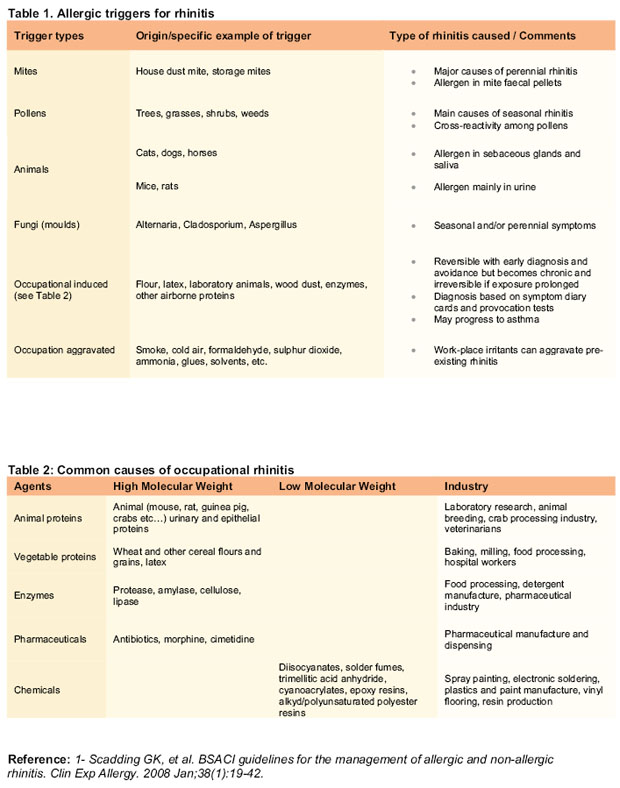
Mar 03, 2011 · Since allergic rhinitis is induced by specific allergens, it makes sense that avoiding those triggers would be an effective treatment. However, this is not always possible as in the case of pollens, and for those with mixed allergic and non-allergic rhinitis, avoidance will not completely alleviate their symptoms.

What will happen if allergic rhinitis is left untreated?
When left untreated, allergic rhinitis often becomes chronic and may lead to complications including: Chronic nasal inflammation and obstruction, which can lead to more serious complications in the airways. Acute or chronic sinusitis. Otitis media, or ear infection.Apr 11, 2018
Can allergic rhinitis last for years?
It clears up on its own after a few days for many people. In others, especially those with allergies, rhinitis can be a chronic problem. Chronic means it is almost always present or recurs often. Rhinitis can last for weeks to months with allergen exposure.
How long does it take to get over allergic rhinitis?
Symptoms of allergic rhinitis have other causes as well, the most customary being the common cold – an example of infectious rhinitis. Most infections are relatively short-lived, with symptoms improving in three to seven days.
Can allergic rhinitis last for weeks?
Allergic rhinitis can last several weeks, longer than a cold or the flu. It does not cause fever. The nasal discharge from hay fever is thin, watery, and clear. Nasal discharge from a cold or the flu tends to be thicker.Apr 2, 2020
How can I permanently cure allergic rhinitis?
There is no cure for allergic rhinitis, but the effects of the condition can be lessened with the use of nasal sprays and antihistamine medications. A doctor may recommend immunotherapy - a treatment option that can provide long-term relief....Typical symptoms of allergic rhinitis include:A runny nose.Sneezing.Itchy eyes.Feb 15, 2022
What is the fastest way to cure allergic rhinitis?
using a short-term course of a decongestant nasal spray to take with your other medication. combining antihistamine tablets with corticosteroid nasal sprays, and possibly decongestants. using a nasal spray that contains a medicine called ipratropium, which will help reduce nasal discharge and make breathing easier.
Why won't my allergies go away?
Unknown Triggers It is possible that you are not entirely sure what is triggering your allergy symptoms, which is why they are not going away. Allergy triggers include pollen, molds, animal dander, and food.May 10, 2020
Which organ is inflamed by rhinitis?
Rhinitis is the medical term for inflammation of the inner lining of the nose. Chronic means that the nasal inflammation is long term, lasting for more than four consecutive weeks.Apr 22, 2019
How do you get rid of allergic rhinitis naturally?
Ginger works as a natural antihistamine, potent antiviral agent, and immune booster. Try some ginger tea to alleviate nasal congestion and headaches. While you sip your tea, inhale the steam coming out of your cup. You can find ginger commercially in fresh and dried form.Oct 15, 2020
Does rhinitis need surgery?
There is no surgical treatment specifically for allergic or nonallergic rhinitis. Surgical treatment revolves around ameliorating symptoms, such as nasal drip and nasal congestion/obstruction.
Why are my allergies getting worse?
The other—and bigger—reason is that many are facing an onslaught of pollen. “With climate change, the general trend has been that we're getting higher levels of pollen and longer pollen seasons, whether that's due to warmer temperatures or increased carbon dioxide emissions; it's probably multifactorial,” says Dr.May 18, 2021
Is allergic rhinitis an autoimmune disease?
Allergic rhinitis is an inflammatory autoimmune disease that causes symptoms such as sneezing, itchy nose, difficulty breathing and/or runny nose (medical term: increased nasal discharge).
How do you know if you have allergic rhinitis?
Common symptoms of allergic rhinitis include: sneezing. a runny nose. a stuffy nose. an itchy nose. coughing. a sore or scratchy throat. itchy eyes. watery eyes.
What are the two types of allergic rhinitis?
What are the types of allergic rhinitis. The two types of allergic rhinitis are seasonal and perennia l. Seasonal allergies usually occur during the spring and fall season and are typically in response to outdoor allergens like pollen. Perennial allergies can occur year round, or at any time during the year in response to indoor substances, ...
What is the most common allergen in seasonal allergic rhinitis?
Pollen is the most common allergen in seasonal allergic rhinitis. These are allergy symptoms that occur with the change of seasons. Nearly 8 percent of adults in the United States experience allergic rhinitis of some kind, according to the American Academy of Allergy, Asthma & Immunology (AAAAI).
How to control allergies indoors?
Using a dehumidifier or a high-efficiency particulate air (HEPA) filter can help you control your allergies while indoors. If you’re allergic to dust mites, wash your sheets and blankets in hot water that’s above 130°F (54.4°C). Adding a HEPA filter to your vacuum and vacuuming weekly may also help.
What is the most common test for allergic reactions?
A skin prick test is one of the most common. Your doctor places several substances onto your skin to see how your body reacts to each one. Usually, a small red bump appears if you’re allergic to a substance. A blood test, or radioallergosorbent test (RAST), is also common.
What is the best treatment for severe allergies?
Immunotherapy. Your doctor may recommend immunotherapy , or allergy shots, if you have severe allergies. You can use this treatment plan in conjunction with medications to control your symptoms. These shots decrease your immune response to particular allergens over time.
How long can you take decongestants for sinuses?
You can use decongestants over a short period, usually no longer than three days, to relieve a stuffy nose and sinus pressure. Using them for a longer time can cause a rebound effect, meaning once you stop your symptoms will actually get worse. Popular OTC decongestants include:
What is the best treatment for allergic rhinitis?
Pharmacologic options for the treatment of allergic rhinitis include intranasal corticosteroids, oral and topical antihistamines, decongestants, intranasal cromolyn (Nasalcrom), intranasal anticholinergics, and leukotriene receptor antagonists. 4, 5 The International Primary Care Respiratory Group, British Society for Allergy and Clinical Immunology, and American Academy of Allergy Asthma and Immunology recommend initiating therapy with an intranasal corticosteroid alone for mild to moderate disease and using second-line therapies for moderate to severe disease. 4 – 7 Patients with moderate to severe disease not responding to oral or topical treatments should be referred for consideration of immunotherapy. 3, 8 Table 2 gives a summary of pharmacologic treatments for allergic rhinitis.
What is immunotherapy for allergic rhinitis?
Immunotherapy should be considered for patients with moderate or severe persistent allergic rhinitis that is not responsive to usual treatments. 8 Targeted immunotherapy is the only treatment that changes the natural course of allergic rhinitis, preventing exacerbation. 39 It consists of a small amount of allergen extract given sublingually or subcutaneously over the course of a few years, with maintenance periods typically lasting between three to five years. The greatest risk associated with immunotherapy is anaphylaxis. Although the usefulness of sublingual immunotherapy in adults with allergic rhinitis has been supported by several large trials, studies in children have met with mixed results, and the FDA has yet to approve a commercial product for sublingual use. 8, 40 – 42
What is allergic rhinitis?
Allergic rhinitis is an immunoglobulin E–mediated disease, thought to occur after exposure to indoor and outdoor allergens such as dust mites, insects, animal danders, molds, and pollens.
What are the effects of antihistamines on the body?
21 The first-generation antihistamines include brompheniramine, chlorpheniramine, clemastine, and diphenhydramine (Benadryl). They may cause substantial adverse effects, including sedation, fatigue, and impaired mental status. These adverse effects occur because the older antihistamines are more lipid soluble and more readily cross the blood-brain barrier than second-generation antihistamines. The use of first-generation antihistamines has been associated with poor school performance, impaired driving, and an increase in automobile collisions and work injuries. 22 – 25 Although one RCT of 63 children eight to 10 years of age did not show that the short-term use of first- or second-generation antihistamines caused drowsiness or impaired school performance, the children in this study were only treated for three days, and the sample size was small. 26
How long does it take for corticosteroids to work?
3 Their onset of action is 30 minutes, although peak effect may take several hours to days, with maximum effectiveness usually noted after two to four weeks of use. 9
Is Nasalcrom safe for allergic rhinitis?
Although safe for general use, intranasal cromolyn (Nasalcrom) is not considered first-line therapy for allergic rhinitis because of its decreased effectiveness at relieving the symptoms of allergic rhinitis and its inconvenient dosing schedule. C. 1, 3.
Can intranasal antihistamines be used for allergic rhinitis?
The adverse effects and higher cost of intranasal antihistamines, as well as their decreased effectiveness compared with intranasal corticosteroids, limit their use as first- or second-line therapy for allergic rhinitis. A.
What is the best treatment for chronic rhinitis?
Immunotherapy, frequently referred to as allergy shots, is a great option for patients with chronic allergic rhinitis. The effects of immunotherapy are long lasting and can help reduce unnecessary healthcare costs later in life.
How much is lost productivity from allergic rhinitis?
It’s estimated that allergic rhinitis causes more than four million missed days of work each year—that’s nearly $700 million in lost productivity. Allergies also account for almost $14.5 billion in annual medical costs. When left untreated, allergic rhinitis often becomes chronic and may lead to complications including: ...
How much did it cost to treat allergic rhinitis in 2000?
In 2000, the average out-of-pocket cost for a patient to treat allergic rhinitis was roughly $1200, but research shows that treating allergic rhinitis through immunotherapy cost patients roughly a third less for the first year of treatment. Treatment in following years was significantly less expensive.
What are the benefits of immunotherapy?
In addition to cost savings, other benefits of immunotherapy include: 1 Improved mood: Because symptoms of allergies can cause fatigue, headaches and irritability, treating those allergies through immunotherapy can help you feel better physically, which helps you feel better mentally and emotionally. 2 No side effects: Unlike over-the-counter medications for allergies, immunotherapy does not cause side effects like drowsiness. It also doesn’t interact with other medications. 3 Less frequent treatment: In the beginning phases of immunotherapy, you may need to get injections several times a month, but throughout the remainder of the treatment, your shots are once per month compared to daily medication. 4 Long-lasting results: Immunotherapy treatment can last up to 20 years in some patients, whereas even a few missed doses of allergy treatments can make symptoms worse. 5 Improved immune system: In addition to treating your current allergies, immunotherapy helps prevent the development of new allergies in the future. It also decreases the chances of developing other allergy-related diseases such as asthma.
Why is immunotherapy important?
In addition to cost savings, other benefits of immunotherapy include: Improved mood: Because symptoms of allergies can cause fatigue, headaches and irritability, treating those allergies through immunotherapy can help you feel better physically, which helps you feel better mentally and emotionally.
How long does immunotherapy last?
Long-lasting results: Immunotherapy treatment can last up to 20 years in some patients, whereas even a few missed doses of allergy treatments can make symptoms worse. Improved immune system: In addition to treating your current allergies, immunotherapy helps prevent the development of new allergies in the future.
What happens if you leave rhinitis untreated?
When left untreated, allergic rhinitis often becomes chronic and may lead to complications including: Chronic nasal inflammation and obstruction, which can lead to more serious complications in the airways. Acute or chronic sinusitis. Otitis media, or ear infection. Sleep apnea or other sleep disturbances. Upper respiratory tract infection.
How to keep your nose from irritating?
Rinse your nasal passages. Use a specially designed squeeze bottle — such as the one included in saline kits — a bulb syringe or a neti pot to irrigate your nasal passages. This home remedy, called nasal lavage, can help keep your nose free of irritants.
What is the best nasal spray for asthma?
Anti-drip anticholinergic nasal sprays. The prescription drug ipratropium is often used as an asthma inhaler medication. But it's now available as a nasal spray and can be helpful if a runny, drippy nose is your main complaint. Side effects can include nosebleeds and drying of the inside of your nose. Decongestants.
What is the test called for examining the inside of the nose?
Nasal endoscopy. This test involves looking at the inside of your nasal passages with a thin, fiber-optic viewing instrument called an endoscope. Your doctor will pass the fiber-optic endoscope through your nostrils to examine your nasal passages and sinuses. CT scan.
What test is needed for sinuses?
If your doctor suspects a sinus problem, you might need an imaging test to view your sinuses. Nasal endoscopy.
Can a doctor test for rhinitis?
Your doctor will perform a physical exam and ask questions about your symptoms. He or she might recommend certain tests, although there are no definite tests for nonallergic rhinitis. Your doctor is likely to decide that you have nonallergic rhinitis if you have nasal congestion, a runny nose or postnasal drip and tests for other conditions don't ...
Can allergies cause rhinitis?
In many cases, rhinitis is caused by an allergic reaction. The only way to be sure rhinitis isn't caused by allergies is through allergy testing, which may involve skin or blood tests.
Can ipratropium be used as a nasal spray?
The prescription drug ipratropium is often used as an asthma inhaler medication. But it's now available as a nasal spray and can be helpful if a runny, drippy nose is your main complaint. Side effects can include nosebleeds and drying of the inside of your nose. Decongestants.

Treatment
Prevention
- Prevention has been a main focus in studies of allergic rhinitis, but few interventions have been proven effective. Although evidence does not support measures to avoid dust mites, such as mite-proof impermeable mattresses and pillow covers, many guidelines continue to recommend them.2,3,6 Other examples of proposed interventions without documented effectiveness includ…
Safety
- There is no evidence that one intranasal corticosteroid is superior. However, many of the products have different age indications from the U.S. Food and Drug Administration (FDA), only budesonide (Rhinocort Aqua) has an FDA pregnancy category B safety rating, and only fluticasone furoate (Flonase) and triamcinolone acetonide are available over the counter.
Adverse effects
- The most common adverse effects of intranasal corticosteroids are throat irritation, epistaxis, stinging, burning, and nasal dryness.2,22 Although there has been concern about potential systemic adverse effects, including the suppression of the hypothalamic-pituitary axis, these effects have not been shown with currently available intranasal corticosteroids.23,24 The studie…
Mechanism
- Histamine is the most studied mediator in early allergic response. It causes smooth muscle constriction, mucus secretion, vascular permeability, and sensory nerve stimulation, resulting in the symptoms of allergic rhinitis.
Pharmacology
- Oral and intranasal decongestants improve nasal congestion associated with allergic rhinitis by acting on adrenergic receptors, which causes vasoconstriction in the nasal mucosa, decreasing inflammation.2,12,13 The most common decongestants are phenylephrine, oxymetazoline (Afrin), and pseudoephedrine. The abuse potential for pseudoephedrine should be weighed against its b…
Research
- Although evidence supports the use of intranasal ipratropium (Atrovent) for severe rhinorrhea, one study showed that it may also improve congestion and sneezing in children, but to a lesser extent than intranasal corticosteroids.35 Adverse effects include dryness of the nasal mucosa, epistaxis, and headache, and the recommended administration is two to three times daily.1
Administration
- Subcutaneous injections are administered in the physician's office at regular intervals, typically three times per week during a buildup phase, then every two to four weeks during a maintenance phase. The first dose of sublingual immunotherapy is administered in the physician's office so that the patient can be observed for adverse effects, and then it is administered at home daily. T…
Other sources
- 1. Nelson HS, Rachelefsky GS, Bernick J. The Allergy Report. Milwaukee, Wis.: American Academy of Allergy, Asthma, and Immunology; 2000....
Treatment
Medical uses
Safety
Adverse effects
Pharmacology
Mechanism of action
- Many studies have demonstrated that nasal corticosteroids are more effective than oral and intranasal antihistamines in the treatment of allergic rhinitis.4,5,1012 One randomized controlled trial (RCT) looking at quality-of-life measures compared the antihistamine loratadine (Claritin) with the nasal corticosteroid fluticasone (Flonase) in 88 adults over a four-week period.13 The study'…
Research
- Although there is no evidence that one intranasal corticosteroid is superior to another, many of the available products have different age indications from the U.S. Food and Drug Administration (FDA). Only budesonide (Rhinocort) carries the FDA pregnancy category B safety rating, and only mometasone (Nasonex) has a delivery device that received recognition from the National Arthrit…
Mechanism
- The adverse effects most commonly experienced with the use of intranasal corticosteroids are headache, throat irritation, epistaxis, stinging, burning, and nasal dryness.3,15 Although the use of intranasal corticosteroids has raised concern for potential systemic adverse effects, including the suppression of the hypothalamic-pituitary axis, the products currently available have not been sh…
Prevention
- Oral and topical decongestants improve the nasal congestion associated with allergic rhinitis by acting on adrenergic receptors, which causes vasoconstriction in the nasal mucosa, resulting in decreased inflammation.35 Although the most commonly available decongestants are phenylephrine, oxymetazoline (Afrin), and pseudoephedrine, the abuse potential for pseudoephe…
Other sources
- Intranasal cromolyn is available over the counter and is thought to act by inhibiting the degranulation of mast cells.1 Although safe for general use, it is not considered first-line therapy for allergic rhinitis because of its decreased effectiveness at relieving symptoms compared with antihistamines or intranasal corticosteroids, and its inconvenient dosing schedule of three or fo…