Can’t spread TB germs to others. Usually have a positive TB blood test or positive skin test reaction. May develop TB disease if they do not receive treatment for LTBI. People with LTBI do not have symptoms, and they cannot spread TB germs to others.
Full Answer
What influences a patient’s acceptance of LTBI treatment?
Treatment of latent TB infection is essential to controlling TB in the United States because it substantially reduces the risk that latent TB infection will progress to TB disease. In the United States, up to 13 million people may have latent TB infection, according to estimates from the U.S. Centers for Disease Control and Prevention (CDC).
When to start anti-TNF therapy after LTBI?
Treatment of latent TB infection is essential to controlling TB in the United States because it substantially reduces the risk that latent TB infection will progress to TB disease. In the United States, up to 13 million people may have latent TB infection.
Can LTBI treatment reduce the risk of TB disease by 90%?
Dec 15, 2017 · In one experimental study with LTBI mouse model, the proportions of mice with positive spleen culture which was done at 6 months after treatment with each regimen (6H, 3 months of rifampin [3R], 2 months of rifampin plus pyrazinamide [2RZ], or 2 months of isoniazid plus rifampin plus pyrazinamide) were 100%, 60%, 56%, and 95%, respectively, suggesting that …
Is diagnostic test necessary for LTBI?
Finally, our results neither support nor refute the idea that a positive IGRA result, in the absence of treatment for LTBI, is associated with a higher risk of reactivation of LTBI, compared with a positive tuberculin skin test result alone. Only long-term follow-up of large numbers of persons will be able to address this topic.

Does TB test positive after treatment?
How do you know if TB treatment is working?
Will latent TB always test positive?
What happens after tuberculosis treatment?
Is TB curable today?
When does TB treatment start working?
Is latent TB gone after treatment?
Can latent TB become active even after treatment?
Does latent TB go away after treatment?
Can TB be treated with LTBI?
Persons with no known risk factors for TB may be considered for treatment of LTBI if they have either a positive IGRA result or if their reaction to the TST is 15 mm or larger. However, targeted TB testing programs should only be conducted among high-risk groups.
Can latent TB be treated?
For this reason, people with latent TB infection should be treated to prevent them from developing TB disease.
Can TB spread to others?
People with latent TB infection do not have symptoms, and they cannot spread TB bacteria to others. However, if latent TB bacteria become active in the body and multiply, the person will go from having latent TB infection to being sick with TB disease.
Why is latent TB important?
Treatment of latent TB infection is essential to controlling TB in the United States because it substantially reduces the risk that latent TB infection will progress to TB disease.
How many people have latent TB?
In the United States, up to 13 million people may have latent TB infection. Without treatment, on average 1 in 10 people with latent TB infection will get sick with TB disease in the future. The risk is higher for people with HIV, diabetes, or other conditions that affect the immune system.
How many people will get TB in the future?
Without treatment, on average 1 in 10 people with latent TB infection will get sick with TB disease in the future. The risk is higher for people with HIV, diabetes, or other conditions that affect the immune system.
Where is TB common?
From countries where TB is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, and Guatemala, or other countries with high rates of TB. (Of note, people born in Canada, Australia, New Zealand, or Western and Northern European countries are not considered at high risk for TB infection, unless they spent time in a country ...
How is acceptance of LTBI influenced?
A patient’s acceptance of LTBI treatment is often influenced by the initial approach of the health care provider. When discussing the risks and benefits of treatment it is important to explain that
What is LTBI in healthcare?
Latent tuberculosis infection (LTBI) is the presence of M. tuberculosis organisms (tubercle bacilli) without symptoms or radiographic or bacteriologic evidence of TB disease. Approximately 90-95% of those infected are able to mount an immune response that halts the progression from LTBI to TB disease. However, because prevention of TB has major public health implications, the Centers for Disease Control and Prevention (CDC) and the United States Preventive Services Task Force (USPSTF) recommend testing populations that are at increased risk for TB infection and treating those for whom TB disease has been ruled out. Health care providers must communicate the risks and benefits of treatment to their patients and encourage adherence and treatment completion.
What is LTBI in TB?
Latent tuberculosis infection (LTBI) is the presence of M. tuberculosis organisms (tubercle bacilli) without symptoms or radiographic or bacteriologic evidence of TB disease. Approximately 90-95% of those infected are able to mount an immune response that halts the progression from LTBI to TB disease. However, because prevention of TB has major ...
How many drugs are needed for TB?
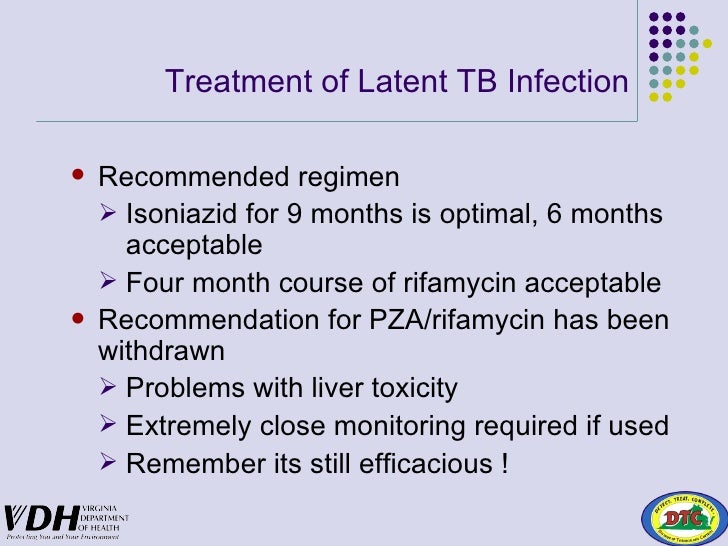
TB infection is treated with one or two drugs, whereas TB disease initially requires four drugs.
What are incentives for patients?
Incentives, which are small rewards that encourage or motivate patients . Local businesses and organizations may be a resource for incentives such as grocery store vouchers, nutritional supplements, movie tickets, or restaurant coupons.
Can TB cause disease?
When discussing the risks and benefits of treatment it is important to explain that. As long as TB germs are in the body, they can begin to multiply and cause disease. Certain individuals are at especially high risk for progression to TB disease.
Can LTBI spread to others?
People with LTBI do not have symptoms, and they cannot spread TB germs to others. However, if latent TB germs become active in the body and multiply, the person will go from having LTBI to being sick with TB disease. For this reason, people with LTBI should be treated to prevent them from developing TB disease.
How many people with LTBI will develop TB?
While not everyone with LTBI will develop TB disease, about 5–10% will develop TB disease over their lifetimes if not treated. Progression from untreated LTBI to TB disease is estimated to account for approximately 80% of U.S. TB cases. Some people who have LTBI are more likely to develop TB disease than others.
What is the cause of TB?
Tuberculosis (TB) is caused by bacteria called Mycobacterium tuberculosis (M. tuberculosis). The bacteria, or germ, usually attack the lungs. TB germs can attack any part of the body, such as the kidney, spine, or brain. There is good news. People with TB can be treated if they seek medical help.
Is TB worse among minorities?
While the number of TB cases in the United States has gone down, TB still has worse effects among racial and ethnic minorities. This is because certain minority groups are more likely to have TB risk factors that can increase the chance of developing the disease (see page 8). This booklet answers common questions about TB.
How does TB spread?
The TB germs are spread into the air when a person with infectious TB disease of the lungs or throat coughs, speaks, or sings. People nearby may breathe in these TB germs and become infected. When a person breathes in TB germs, the TB germs can settle in the lungs and begin to grow.
Where is TB common?
People who were born in or who frequently travel to countries where TB disease is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, Guatemala, and other countries with high rates of TB.
Can TB be inactive?
In most people who breathe in TB germs and become infected, the body is able to fight the TB germs to stop them from growing. The TB germs become inactive, but they remain alive in the body and can wake up and become active later. This is called latent TB infection, or LTBI for short. People with LTBI.
Is TB inactive or alive?
Has TB bacteria in his/her body that are alive, but inactive. Needs treatment for latent TB infection to prevent TB disease; however, if exposed and infected by a person with multidrug-resistant TB (MDR TB) or extensively drug-resistant TB (XDR TB), preventive treatment may not be an option.
Can TB be treated with XDR?
Needs treatment for latent TB infection to prevent TB disease; however, if exposed and infected by a person with multidrug-resistant TB (MDR TB) or extensively drug-resistant TB (XDR TB), preventive treatment may not be an option.
What are the symptoms of TB?
What is TB Disease? 1 Coughing for 3 weeks or longer 2 Hemoptysis (coughing up blood) 3 Chest pain
Can TB be spread to others?
The only sign of TB infection is a positive reaction to the tuberculin skin test or TB blood test. Persons with latent TB infection are not infectious and cannot spread TB infection to others. Overall, without treatment, about 5 to 10% of infected persons will develop TB disease at some time in their lives.
What is XDR TB?
Of special concern are persons infected by someone with extensively drug-resistant TB (XDR TB) who later develop TB disease; these persons will have XDR TB, not regular TB disease. Usually has a skin test or blood test result indicating TB infection. Has TB bacteria in his/her body that are alive, but inactive.
How does TB affect the immune system?
In some people, TB bacteria overcome the defenses of the immune system and begin to multiply, resulting in the progression from latent TB infection to TB disease. Some people develop TB disease soon after infection, while others develop TB disease later when their immune system becomes weak. The general symptoms of TB disease include. ...
How long does it take for TB to cause coughing?
Unexplained weight loss. Loss of appetite. Night sweats. Fever. Fatigue. Chills. The symptoms of TB of the lungs include. Coughing for 3 weeks or longer.
Is LTBI treatment protective?
No LTBI treatment is completely protective against reactivation. INH-based regimens, for example, reduce the incidence of reactivation by about 75%. 35–37 The direct impact of LTBI treatment on preventing TB reactivation in the setting of biologic therapy, especially in IBD patients, has not been extensively studied.
What is LTBI treatment?
Treatment for latent tuberculosis infection (LTBI) is of particular concern in patients with inflammatory bowel disease (IBD) initiating biologic therapies to prevent tuberculosis (TB) reactivation. This study aimed to evaluate the effectiveness of LTBI treatment in IBD patients receiving biologic therapy.
When did IBD patients receive biologic therapy?
There was a retrospective review of all IBD patients diagnosed with LTBI following a tuberculin skin test (TST) and/or interferon gamma release assay (IGRA) and who received biologic therapy between 2002 and 2016. The primary outcome was tuberculosis reactivation after completion of LTBI treatment.
What are the immunologic therapies for UC?
The treatment of inflammatory bowel diseases (IBD), such as ulcerative colitis (UC) and Crohn’s Disease (CD), was revolutionized by the development of targeted immunologic therapies (“biologics”) against tumor necrosis factor alpha (TNF-α), integrins, and interleukins. 1, 2 One significant risk of using these newer therapies is an increased risk of infection; specifically, reactivation of latent tuberculosis infections (LTBI) in patients on biologic medications. 3–5 TNF-α has a role in recruiting inflammatory cells to sites of infection, enhancing phagocytosis, and aids in the development and maintenance of granulomas. 6–8 Hence, the impairment of these immune pathways increases the risk of reactivation of LTBI in patients taking anti-TNF-α agents. 6–8 The risk of LTBI reactivation in patients taking anti-integrin medications does not seem to carry the same risk as patients taking anti-TNF-α agents, as a recent meta-analysis showed only 1 case of tuberculosis (TB) in 1 of 643 patients. 9