
What are the treatment medications for active tuberculosis?
- Take your medicine exactly as the healthcare provider directed.
- When you cough, sneeze or laugh, cover your mouth with a tissue. ...
- Do not go to work or school until your healthcare provider says it's okay.
- Avoid close contact with anyone. ...
- Air out your room often so the TB germs don't stay in the room and infect someone else.
What are the phases of TB treatment?
The following are the stages of TB:
- Exposure. This happens when a person has been in contact with, or exposed to, another person who has TB. ...
- Latent TB infection. This happens when a person has TB bacteria in his or her body, but does not have symptoms of the disease. ...
- TB disease. This describes the person who has signs and symptoms of an active infection. ...
What medications are used to treat TB?
What is the treatment for TB?
- The following medications are commonly used to treat TB:
- Isoniazid. Each small white tablet contains 100mg of Isoniazid and the adult dose is 300mg daily. ...
- Rifampicin. The capsules come in two strengths, 150mg or 300mg. The colours vary with the different brands and strengths.
What is the best treatment for latent TB?
Treatment of LTBI and TB for Persons with HIV
- Latent TB Infection and HIV. Someone with untreated latent TB infection and HIV infection is much more likely to develop TB disease during his or her lifetime than someone without ...
- TB Disease and HIV. ...
- Drug-Resistant TB and HIV. ...
- Antiretroviral Therapy During TB Treatment. ...
- Drug Interactions. ...
- Case Management. ...
What is the WHO recommended treatment protocol for TB?
The preferred regimen for treating adults with TB remains a regimen consisting of an intensive phase of 2 months of isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB) followed by a continuation phase of 4 months of INH and RIF.
Is treatment for active TB required?
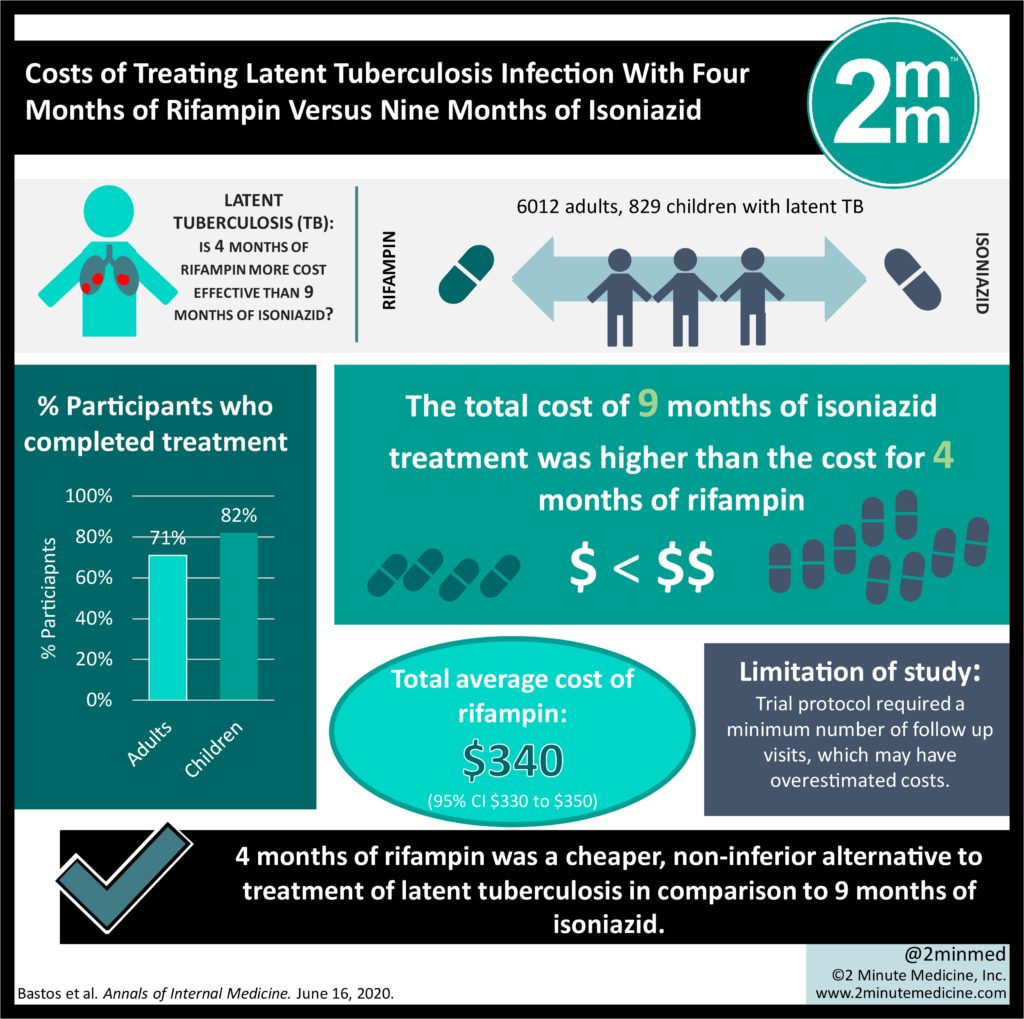
If you have latent TB , your doctor might recommend treatment with medication if you're at high risk of developing active TB . For active tuberculosis, you must take antibiotics for at least six to nine months.
What is the most common treatment for active TB?
The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB takes much longer than other bacterial infections.
Do active TB patients need to be isolated?
Patients with confirmed infectious TB or those being evaluated for active TB disease should be kept in airborne isolation precautions until active TB disease is ruled out or the patient is deemed to be noninfectious.
Does active TB require hospitalization?
Most people may remain at home, but all should be kept from any new contacts for at least 2 weeks after treatment begins. The elderly and those who are acutely ill or have multidrug resistant TB should be hospitalized for the first few weeks of treatment.
What is the quarantine period for TB?
Note: Home isolation is recommended for the initial three to five days of appropriate four-drug TB treatment.
What is considered active TB?
TB bacteria become active if the immune system can't stop them from growing. When TB bacteria are active (multiplying in your body), this is called TB disease. People with TB disease are sick. They may also be able to spread the bacteria to people they spend time with every day.
When is active TB no longer contagious?
Although tuberculosis is contagious, it's not easy to catch. You're much more likely to get tuberculosis from someone you live or work with than from a stranger. Most people with active TB who've had appropriate drug treatment for at least two weeks are no longer contagious.
What is the duration of TB treatment?
RIPE regimens for treating TB disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment). This is the preferred regimen for patients with newly diagnosed pulmonary TB.
When can a TB patient be discharged?
a) The patient has completed and tolerated at least 14 days of appropriate multi-drug TB treatment that is consistent with CDPH/CTCA Guidelines for the Treatment of Tuberculosis and Tuberculosis Infection and exhibits clinical improvement (e.g., reduction in fever or cough).
What type of precautions need to be applied for clients with active TB?
Personal protective equipment is part of the airborne precautions protocol. All patients with suspected or confirmed active (infectious) TB should be directly admitted to the health care facility, bypassing the ER and immediately be put on airborne precautions in a negative pressure airborne isolation room.
What are the 3 stages of tuberculosis?
There are 3 stages of TB—exposure, latent, and active disease. A TB skin test or a TB blood test can diagnose the disease. Treatment exactly as recommended is necessary to cure the disease and prevent its spread to other people.
How long does it take to treat TB?
TB disease can be treated by taking several drugs for 6 to 9 months. There are 10 drugs currently approved by the U.S. Food and Drug Administration (FDA) for treating TB. Of the approved drugs, the first-line anti-TB agents that form the core of treatment regimens are: isoniazid (INH) rifampin (RIF)
What is it called when TB bacteria multiply?
When TB bacteria become active (multiplying in the body) and the immune system can’t stop the bacteria from growing, this is called TB disease. TB disease will make a person sick. People with TB disease may spread the bacteria to people with whom they spend many hours.
What is XDR TB?
Extensively drug-resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin). Treating and curing drug-resistant TB is complicated.
Can TB be treated?
It is very important that people who have TB disease are treated, finish the medicine, and take the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again; if they do not take the drugs correctly, the TB bacteria that are still alive may become resistant to those drugs.
Is TB a serious disease?
TB is a serious disease, and can be fatal if not treated properly. It is important to remember that all medications have risks and benefits. Learn more from CDC’s Dear Colleague letter. Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and TB disease.
Can rifampin be used for TB?
Treatment. impurities in rifampin and rifapentine, two important anti-tuberculosis (TB) medications. People with TB disease or latent TB infection taking rifampin or rifapentine should continue taking their current medication, and should talk with their healthcare provider about any concerns.
What is the treatment of tuberculosis?
Treatment of tuberculosis is focused on both curing the individual patient and minimizing the transmission of Mycobacterium tuberculosis to other persons; successful treatment of tuberculosis has benefits both for the individual patient and the community in which the patient resides.
What is the decision to initiate combination chemotherapy for tuberculosis?
The decision to initiate combination chemotherapy for tuberculosis is based on clinical, radiographic, laboratory, patient, and public health factors (Figure 1). In addition, clinical judgment and the index of suspicion for tuberculosis are critical in making a decision to initiate treatment.
What is the ATS guideline?
The American Thoracic Society (ATS), Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) jointly sponsored the development of this guideline on the treatment of drug-susceptible tuberculosis, which is also endorsed by the European Respiratory Society (ERS) and the US National Tuberculosis Controllers Association (NTCA). This guideline provides recommendations on the clinical and public health management of tuberculosis in children and adults in settings in which mycobacterial cultures, molecular and phenotypic drug susceptibility tests, and radiographic studies, among other diagnostic tools, are available on a routine basis. Nine PICO (population, intervention, comparators, outcomes) questions and associated recommendations, developed based on the evidence that was appraised using GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology [1, 2], are summarized below. A carefully selected panel of experts, screened for conflicts of interest, including specialists in pulmonary medicine, infectious diseases, pharmacokinetics, pediatrics, primary care, public health, and systematic review methodology were assembled and used GRADE methods to assess the certainty in the evidence (also known as the quality of evidence) and strength of the recommendations (see Supplementary Appendix A: Methods and Table 1). This executive summary is a condensed version of the panel's recommendations. Additional detailed discussion of the management of pulmonary and extrapulmonary tuberculosis is available in the full-text version of this guideline.
Is co-trimoxazole used for HIV?
Whereas the WHO recommends routine co-trimoxazole prophylaxis for all HIV-infected people with active tuberculosis disease regardless of the CD4 cell count [66], in high-income countries, co-trimoxazole prophylaxis is primarily used in tuberculosis patients coinfected with HIV with CD4 counts <200 cells/µL [67].
Diagnosis
- In July 2021, WHO released the WHO consolidated guidelines on tuberculosis. Module 3: Diagnosis – rapid diagnostics for tuberculosis detection 2021 update (3).Three new classes of nucleic acid amplification test (NAAT) are now endorsed by WHO: 1. moderate complexity auto…
Treatment
- In April 2021, WHO convened a guideline development group (GDG) to review data from a trial conducted in 13 countries that compared 4-month rifapentine-based regimens with a standard 6-month regimen in people with drug-susceptible TB (6). The GDG considereda 4-month regimen composed of rifapentine, isoniazid, pyrazinamide and moxifloxacin that met the non-inferiority c…
Comorbidities, Vulnerable Populations and People-Centred Care
- In May to June 2021, WHO convened a GDG to review updated evidence on the management of TB in children and adolescents (aged 0–9 and 10–19 years, respectively). A rapid communication thatsummarizes the main updates to guidance on the management of TB in children and adolescents was released by WHO in August 2021 (8). The communication includes new inform…
Other Actions to Support TB Policy Guidance
- To exchange views on emerging areas where there is a need for global TB policy guidance, in March 2021, WHO convened a consultation on the translation of TB research into global policy guidelines, attended by scientists, public health experts, partners,civil society and countries (9). In June 2021, WHO launched a TB Knowledge Sharing Platform to bring all WHO TB guidelines, op…