
Full Answer
What is Botox for achalasia?
Botulinum Toxin (Botox®) Injection for Achalasia Botulinum toxin is a naturally occurring protein produced by the bacterium Clostridium botulinum. Injection of botulinum toxin into muscles causes temporary paralysis of the specific muscle, which lasts for months to over one year.
Is botulinum toxin effective for esophageal achalasia?
Botulinum toxin injection for esophageal achalasia is also useful in Japanese patients, as reported in western countries. However, some studies have reported that most patients who are treated with botulinum toxin injection experience relapse, usually 6–12 months after the first treatment, and often require repeated treatment.
What is achalasia and how is it treated?
Treatment of achalasia with botulinum A toxin Achalasia is an idiopathic neuromuscular disorder of the esophagus which is associated with absence of esophageal peristalsis and incomplete relaxation of a normal or raised lower esophageal sphincter (LES). Dysphagia is the most commonly associated symptom. Conventional therapeutic approaches are d …
What is the treatment for esophageal achalasia in Japan?
In Japan, esophageal achalasia has been treated with oral drugs, endoscopic balloon dilation, per-oral endoscopic myotomy (POEM), and surgery. However, local injection of botulinum toxin for esophageal achalasia has not been approved as a treatment for medical insurance in Japan.
Where do you inject Botox for achalasia?
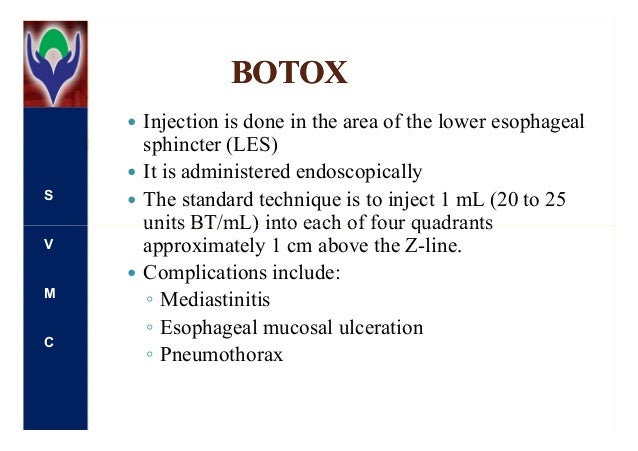
Injection of botulinum toxin into muscles causes temporary paralysis of the specific muscle, which lasts for months to over one year. In gastroenterology, botulinum toxin is used primarily to treat achalasia. Botulinum toxin is injected into the muscle of the lower esophageal sphincter.
How does Botox treat achalasia?
The concept behind botulinum toxin injection for achalasia is that it addresses this imbalance by blocking acetylcholine release from excitatory neurones acting on the lower esophageal sphincter. This results in a decrease in lower esophageal sphincter tone that can allow improved esophageal emptying.
Which sphincter is affected by achalasia?
With achalasia, your lower esophageal sphincter (LES) fails to open up during swallowing. This muscular ring closes off your esophagus from your stomach most of the time, but it opens when you swallow so food can pass through.
What does the injection of botulinum toxin into the LES do?
Endoscopic injection technique of botulinum toxin As botulinum toxin (botox) is a potent inhibitor of acetylcholine release from nerve endings, it counteracts the unopposed LES contraction mediated by cholinergic nerves, thereby lowering LES pressure.
How does Botox work in the esophagus?
Botulinum toxin injections (Botox®) offer a safe alternative to patients with advanced esophagus disorders who can't have or don't want a minimally invasive procedure. Botox® injections work by interfering with nerve signals to the muscle tissue in your esophagus and releasing an enzyme to help them relax.
What is the mechanism of action of Botox?
Botulinum toxin acts by binding presynaptically to high-affinity recognition sites on the cholinergic nerve terminals and decreasing the release of acetylcholine, causing a neuromuscular blocking effect. This mechanism laid the foundation for the development of the toxin as a therapeutic tool.
What is the best treatment for achalasia?
Laparoscopic Heller Myotomy and Fundoplication The most effective treatment for achalasia is Heller myotomy (esophagomyotomy), a procedure in which the muscle fibers of the lower esophageal sphincter (LES) are divided.
What causes the lower esophageal sphincter to open?
The lower esophageal sphincter remains closed except for when you swallow. Then, it opens to allow food to move down into the stomach. When you swallow, several structures react to block the airways, so food particles don't get into your lungs. Food enters the throat, and then both esophageal sphincters open.
What is the pathophysiologic mechanism of achalasia?
Pathophysiologically, achalasia is caused by loss of inhibitory ganglion cells in the myenteric plexus. Since the initial description, several studies have attempted to explore initiating agents that may cause the disease such as viral infection, other environmental factors, autoimmunity, and genetic factors.
How do you mix Botox for achalasia?
Reconstitute two 100 Unit vials of BOTOX, each with 6 mL of preservative-free 0.9% Sodium Chloride Injection, USP and mix the vials gently. Draw 4 mL from each vial into each of two 10 mL syringes. Draw the remaining 2 mL from each vial into a third 10 mL syringe for a total of 4 mL in each syringe.
Does Botox inhibit gastric reflux?
Botox injection into the lower esophageal sphincter induces hiatal paralysis and gastroesophageal reflux.
Can esophageal dysphagia be treated with Botox?
Botox can sometimes be used to treat achalasia, a condition where the muscles in the oesophagus become too stiff to allow food and liquid to enter the stomach. Botox can be used to paralyse the tightened muscles that prevent food from reaching the stomach.
What is the treatment for achalasia?
Patients with difficulty swallowing due to achalasia may be treated with botulinum toxin injection. Alternative treatments include peroral endoscopic myotomy (POEM), Heller myotomy (a traditional surgery), and pneumatic dilation. Botulinum toxin may also be injected into the upper esophageal sphincter to treat other types of difficulty swallowing, ...
How long before botulinum toxin injection for achalasia?
Preparation for botulinum toxin injection for achalasia is similar to preparation for upper endoscopy, except you should limit your diet to liquids for at least 24 hours before the procedure.
How long does it take for botulinum toxin to work?
The results of the procedure will be communicated to your referring physician (s). It can take a few days to a week before you notice the effects of botulinum toxin. The effects are not permanent, so re-injections are typically needed months later.
What is botox injection?
Botulinum Toxin (Botox®) Injection for Achalasia. Botulinum toxin is a naturally occurring protein produced by the bacterium Clostridium botulinum. Injection of botulinum toxin into muscles causes temporary paralysis of the specific muscle, which lasts for months to over one year.
Where is botulinum toxin injected?
In gastroenterology, botulinum toxin is used primarily to treat achalasia. Botulinum toxin is injected into the muscle of the lower esophageal sphincter.
Is botulinum toxin injection safe?
Botulinum toxin injection is generally a very safe procedure. Very rare complications include bleeding and infection. If you notice blood in your stool, black stool, fever, chills, vomiting, chest pain, stomach pain, or shortness of breath, contact your doctor as instructed on your discharge papers.
What is the procedure to treat achalasia?
Surgery. Surgical options for treating achalasia include: Heller myotomy. The surgeon cuts the muscle at the lower end of the esophageal sphincter to allow food to pass more easily into the stomach. The procedure can be done noninvasively (laparoscopic Heller myotomy).
How to treat achalasia?
Surgical options for treating achalasia include: 1 Heller myotomy. The surgeon cuts the muscle at the lower end of the esophageal sphincter to allow food to pass more easily into the stomach. The procedure can be done noninvasively (laparoscopic Heller myotomy). Some people who have a Heller myotomy may later develop gastroesophageal reflux disease (GERD).#N#To avoid future problems with GERD, a procedure known as fundoplication might be performed at the same time as a Heller myotomy. In fundoplication, the surgeon wraps the top of your stomach around the lower esophagus to create an anti-reflux valve, preventing acid from coming back (GERD) into the esophagus. Fundoplication is usually done with a minimally invasive (laparoscopic) procedure. 2 Peroral endoscopic myotomy (POEM). In the POEM procedure, the surgeon uses an endoscope inserted through your mouth and down your throat to create an incision in the inside lining of your esophagus. Then, as in a Heller myotomy, the surgeon cuts the muscle at the lower end of the esophageal sphincter.#N#POEM may also be combined with or followed by later fundoplication to help prevent GERD. Some patients who have a POEM and develop GERD after the procedure are treated with daily oral medication.
How does achalasia work?
Achalasia treatment focuses on relaxing or stretching open the lower esophageal sphincter so that food and liquid can move more easily through your digestive tract. Specific treatment depends on your age, health condition and the severity of the achalasia.
What is the procedure to remove acid from the stomach?
Fundoplication is usually done with a minimally invasive (la paroscopic) procedure. Peroral endoscopic myotomy (POEM).
Why is achalasia misdiagnosed?
Diagnosis. Achalasia can be overlooked or misdiagnosed because it has symptoms similar to other digestive disorders. To test for achalasia, your doctor is likely to recommend: Esophageal manometry.
How long does Botox last?
Botox injections typically do not last more than six months. A strong improvement from injection of Botox may help confirm a diagnosis of achalasia. Medication.
Can you inject Botox into the esophageal sphincter?
This procedure requires sedation. Botox (botulinum toxin type A). This muscle relaxant can be injected directly into the esophageal sphincter with an endoscopic needle. The injections may need to be repeated, and repeat injections may make it more difficult to perform surgery later if needed.
What is the purpose of endoscopic injection of Botox?
Endoscopic intrasphincteric injection of Botox (ISIB) is used routinely for the treatment of achalasia esophagus and other spastic motor disorders. Studies show that the ISIB reduces the smooth muscle lower esophageal sphincter (LES) pressure.
Does botox help with achalasia?
Botox injection into the lower esophageal sphincter induces hiatal paralysis and gastroesophageal reflux. Endoscopic intrasphincteric injection of Botox (ISIB) is used routinely for the treatment of achalasia esophagus and other spastic motor disorders. Studies show that the ISIB reduces the smooth muscle lower esophageal sphincter (LES) pressure.
What is botox injection?
Botulinum toxin (botox) injection in the esophageal body or lower esophageal sphincter (LES) is considered an effective and low-risk procedure for the short-term relief of symptoms in achalasia and spastic esophageal motility disorders. 1,2 In achalasia patients with advanced age, significant comorbidities or high risk of surgery-related complications, botox injection is often the treatment of choice, since it is considered the safest therapy for this disease. 2–5 It has comparable short-term efficacy, but fewer significant adverse effects than myotomy or dilatation. 3,6 In spastic esophageal motor disorders, botox injection is superior to sham treatment, but the overall efficacy is lower than in achalasia. 1 However, recently, a fatal mediastinitis following esophageal botulinum toxin injection has been reported, 7 raising the question whether this treatment is really as safe as we think.
When was botulinum toxin first used?
Esophageal injection of botulinum toxin was first described in 1993 in a patient with therapy-resistant achalasia. 8 Botulinum toxin, a purified neurotoxin complex, inhibits acetylcholine release from cholinergic neurons, preventing neuromuscular conduction.
What are the complications of a clavien-dindo?
A total of 52 (7.9%) mild complications (Clavien-Dindo grade I) were reported by 48 patients, consisting of chest pain or heartburn in 29 procedures, epigastric pain in five procedures, vertigo, nausea or vomiting in four procedures, acute urinary retention requiring bladder catheterization in one procedure and other mild complications of fatigue, sore throat, dyspnoea, or vomiting in 9 procedures (Table 3 ). No complications of ulceration, perforation, pneumothorax, abscess, or heart block were reported . One 64-year-old patient died after developing acute mediastinitis (Clavien-Dindo grade V) following injections of a total of 100 U botulinum toxin in the body of the esophagus for treatment of distal esophageal spasm. Within 1 week he developed a mediastinitis with an abscess between the esophagus and aorta, for which he was treated with intravenous antibiotics and subsequently with surgical drainage of the abscess. After initial symptom relief his condition suddenly deteriorated 3 weeks later. During thoracotomy he died of a ruptured infectious aneurysm of the aorta. Early treatment failure was reported after 85 (25%) procedures. In four patients, the procedure was aborted prematurely. In two patients early termination was due to restlessness, in one patient due to concern for perforation and in one patient due to stasis of food. The distribution of complications is different per diagnosis. Out of 195 treatments for achalasia, 26 (13.3%) procedures led to a complication. Among 141 treatments for spastic disorders (diffuse esophageal spasm, Jackhammer or Nutcracker esophagus), after 23 (16.3%) procedures a complication was reported. After treatment for EGJ outflow obstruction a complication occurred in 2 (8.3%) out of 24 procedures. Treatment for other indications only led to a complication in 1 (4.5%) out of 22 procedures. The type of complication per diagnosis is shown in Figure 1.
Is botox safe for esophageal motility?
In achalasia and spastic esophageal motility disorders, botulinum toxin (botox) injection is considered an effective and low-risk procedure for short-term symptom relief. It is mainly offered to medically high-risk patients. However, no analysis of risks of botox injections has been performed. To determine the incidence and risk factors of procedure-related complications after esophageal botox injections, we analyzed the records of all patients undergoing botox injection therapy for esophageal motility disorders at four university hospitals in Europe and North America between 2008 and 2014. Complications were assigned grades according to the Clavien-Dindo classification. In 386 patients, 661 botox treatments were performed. Main indications were achalasia (51%) and distal esophageal spasm (DES) (30%). In total, 52 (7.9%) mild complications (Clavien-Dindo grade I) were reported by 48 patients, the majority consisting of chest pain or heartburn (29 procedures) or epigastric pain (5 procedures). No ulceration, perforation, pneumothorax, or abscess were reported. One patient died after developing acute mediastinitis (Clavien-Dindo grade V) following injections in the body of the esophagus. In univariate logistic regression, younger age was associated with an increased risk of complications (OR 1.43, 95%CI 1.03–1.96). Treatment for DES, injections into the esophageal body, more injections per procedure, more previous treatments and larger amount of injected botulinum toxin were no risk factors for complications. Esophageal botox injection seems particularly appropriate for high-risk patients due to low complication rate. However, it should not be considered completely safe, as it is associated with rare side effects that cannot be predicted.
Is botulinum toxin safe for achalasia?
We conclude that esophageal botulinum toxin injection is a welcome option in the management of esophageal motility disorders and seems particularly appropriate for medically high-risk achalasia patients due to low risks. However, it is associated with rare side effects that cannot be predicted.
