Positive pressure ventilation with positive end-expiratory pressure (PEEP) set at 5-10 mm Hg may improve oxygenation in patients with noncardiogenic pulmonary edema and allow for lower fraction of inspired oxygen (FIO 2) settings. An FIO 2 greater than 50% for longer than 24 hours may result in oxygen toxicity.
Full Answer
How is pulmonary edema measured on a chest radiograph?
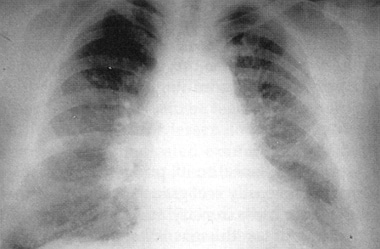
The chest radiograph remains the most practical and useful method of radiologically assessing and quantifying pulmonary edema 3,4. Features useful for broadly assessing pulmonary edema on a plain chest radiograph include: upper lobe pulmonary venous diversion (stag's antler sign)
What are the diagnostic options for pulmonary edema?
Pulmonary edema 1 Pathology. It can arise from a range of cardiogenic and non-cardiogenic causes. 2 Radiographic features. The chest radiograph remains the most practical and useful method... 3 Differential diagnosis.
What is the definition of edema in the lungs?
Pulmonary edema. Pulmonary edema is a broad descriptive term and is usually defined as an abnormal accumulation of fluid in the extravascular compartments of the lung 1.
Which physical findings are characteristic of noncardiogenic pulmonary edema?
Noncardiogenic pulmonary edema shows the classic “batwing” pattern of pulmonary opacities radiating centrifugally from the hila with air bronchogram. Cardiomegaly, pleural effusion, and mediastinal widening are usually not seen. Lung volume may be normal or increased.[2]
What is the treatment for cardiogenic pulmonary edema?
The general treatment of cardiogenic pulmonary edema includes diuretics, possibly morphine and often nitrates. The appropriate use of newer approaches – such as, nesiritide, high-dose vasodilators, milrinone, and vasopressin receptor antagonists – needs larger clinical trials.
What is the initial treatment of pulmonary edema?
The first treatment for acute pulmonary edema is oxygen. Oxygen flows through a face mask or a flexible plastic tube with two openings (nasal cannula) that deliver oxygen to each nostril. This should ease some symptoms. A health care provider monitors the oxygen level.
How is non cardiogenic pulmonary edema treated?
Treatment of noncardiogenic pulmonary edema involves addressing the underlying cause of the event. There are currently no treatment options to address the vascular permeability in ARDS.
What is the best position for a patient with pulmonary edema?
Our results show that the prone position may be a useful maneuver in treating patients with severe hypoxemia due to pulmonary edema. The presence of pulmonary edema, as in early ARDS and HPE predicts a beneficial effect of the prone position on gas exchange.
What is the best medication for edema?
More-severe edema may be treated with drugs that help your body expel excess fluid in the form of urine (diuretics). One of the most common diuretics is furosemide (Lasix).
Which treatment strategy for pulmonary edema is evidence based?
There is a lack of high-quality evidence to guide the treatment of acute pulmonary oedema. The strongest evidence is for nitrates and non-invasive ventilation. Diuretics are indicated for patients with fluid overload. Furosemide (frusemide) should be given by slow intravenous injection.
What is diffuse pulmonary edema?
Pulmonary edema, also known as pulmonary congestion, is excessive liquid accumulation in the tissue and air spaces (usually alveoli) of the lungs. It leads to impaired gas exchange and may cause hypoxemia and respiratory failure.
How can we differentiate between cardiogenic pulmonary edema and non cardiogenic pulmonary edema?
Noncardiogenic pulmonary edema is caused by changes in capillary permeability as a result of a direct or an indirect pathologic insult, while cardiogenic pulmonary edema occurs due to increased capillary hydrostatic pressure secondary to elevated pulmonary venous pressure.
What procedure is done to remove fluid from lungs?
Thoracentesis is a procedure to remove fluid or air from around the lungs. A needle is put through the chest wall into the pleural space. The pleural space is the thin gap between the pleura of the lung and of the inner chest wall.
What happens if you have pulmonary edema?
In general, if pulmonary edema continues, the pressure in the pulmonary artery can rise (pulmonary hypertension). Eventually, the heart becomes weak and begins to fail, and pressures in the heart and lungs go up. Pulmonary edema complications may include: Breathing difficulty.
How does furosemide help pulmonary edema?
Furosemide doubled the pulmonary blood flow in the isolated lobe for the same driving pressure and the greater the amount of lobar edema the less pronounced was this furosemide-associated increase in blood flow.
Which medication is used to decrease afterload in a patient with pulmonary edema?
Milrinone. Milrinone is a positive inotropic agent and vasodilator. It reduces afterload and preload and increases cardiac output.
What is a lung oedema?
Pulmonary oedema. Pulmonary oedema is a broad descriptive term and is usually defined as an abnormal accumulation of fluid in the extravascular compartments of the lung 1.
What are the four main categories of pulmonary oedema?
One method of classifying pulmonary oedema is as four main categories on the basis of pathophysiology which include: increased hydrostatic pressure oedema. two pathophysiological and radiological phases are recognised in the development of pressure oedema. interstitial oedema.
Is pulmonary oedema bilateral or bilateral?
Whether all or only some of these features can be appreciated on the plain chest radiograph, depend on the specific aetiology 1. Furthermore, pulmonary oedema is usually a bilateral process, but it may uncommonly appear to be unilateral in certain situations and pathologies (see unilateral pulmonary oedema ).
What causes pulmonary edema?
In most cases, an increased intravascular pressure due to pulmonary venous hypertension is the predominant cause, resulting in loss of fluid into the interstitium. This may result from left heart failure, left atrial or pulmonary venous obstruction, volume overload in renal failure, or overhydration. Low intravascular oncotic pressure resulting from hypoalbuminemia, liver failure, or renal failure also can result in an increased interstitial transudation of fluid.
What is permeability edema?
Permeability edema is a manifestation of capillary endothelial injury with resultant loss of fluid and protein into the lung interstitium. It results in a high-protein edema and, therefore, is slow to clear. It often is associated with respiratory epithelial injury, and diffuse alveolar damage (DAD). This combination often results in the clinical entities known as acute lung injury (ALI) and the acute respiratoy distress syndrome (ARDS).
What is thickening of the peribronchovascular interstitium?
Thickening of the peribronchovascular interstitium often occurs in patients with interstitial edema, resulting in apparent bronchial wall thickening on chest radiographs, or peribronchial cuffing (see Fig. 11-2 ). Peribronchial cuffing is easiest to recognize in the perihilar regions where bronchi are seen end-on; sometimes lines radiating outward from the hila reflect the thickened peribronchial interstitium. On CT, thickening of the peribronchovascular interstitium resembles bronchial wall thickening; pulmonary arteries adjacent to the bronchi appear increased in diameter because the thickened interstitium surrounds them as well.
What are Kerley's B lines?
Kerley’s B lines visible on chest radiographs result from thickening of interlobular septa ( Fig. 11-1; see also Fig. 10-1 in Chapter 10 ). They are horizontal, 1 to 2 cm in length, touch the pleural surface, and are best seen laterally in the costophrenic angles. Their characteristic appearance results from the regular organization of pulmonary lobules at the lung bases.
What is the poor definition of lower lobe vessels?
Poor definition of lower lobe vessels usually is the first abnormality noted in pulmonary edema and may be seen when Kerley’s lines are unrecognizable. Poor definition of hilar or perihilar vessels is a common finding in patients with mild pulmonary edema ( Fig. 11-3 ). On radiographs, this finding, sometimes referred to as perihilar haze, ...
What are the complications of pulmonary disease?
Common pulmonary complications that occur in critically ill patients include pulmonary edema (hydrostatic; increased capillary permeability), acute lung injury (ALI) and the acute respiratory distress syndrome (ARDS), atelectasis, pneumonia, aspiration, pulmonary embolism, and pulmonary hemorrhage. To some extent, the radiographic distribution of pulmonary disease, the time course of radiographic abnormalities, and associated radiographic findings may help in reaching a useful differential diagnosis. However, the radiographic findings in a patient in the ICU with acute pulmonary disease may be nonspecific, and knowledge of the clinical history or physical findings often is essential in suggesting the appropriate diagnosis.
What percentage of patients in the ICU have radiographs?
Radiographs obtained routinely or following placement of a tube or catheter show significant abnormalities not suspected clinically in 35% to 65% of patients in the ICU, and these findings often result in an intervention or change in treatment. The American College of Radiology ( www.acr.org) recommends daily portable radiographs in patients ...
What tests are done to diagnose pulmonary disease?
Blood tests, pulmonary function tests (spirometry), pulse oximetry, chest x-ray, chest CT, bronchoscopy with biopsy, or surgical biopsy may be performed to help diagnose your condition. Treatment may depend on the underlying cause of the disease and your health status. Medication, respiratory therapy or surgery may be prescribed to help improve ...
What tests are performed to determine if a patient has interstitial lung disease?
To determine the cause of interstitial lung disease, a physician may perform a physical examination and order diagnostic tests, including: Blood tests: These tests may help identify autoimmune diseases, such as scleroderma and rheumatoid arthritis, which can be associated with interstitial lung disease.
What happens when the alveoli are inflamed?
When affected by an interstitial lung disease, the tissue supporting the alveoli becomes inflamed and stiff, which makes it difficult for the alveoli to fully expand. The abnormal interstitium limits the delivery of oxygen to the body and the removal of carbon dioxide from the body. As interstitial disease progresses, ...
What is the test of lung function?
Spirometry: This is a test of lung function, in which the patient exhales quickly and forcefully through a tube connected to a machine that measures how much air the lungs can hold and how quickly the air moves in and out of the lungs.
How does oxygen enter the alveoli?
In a normal lung, the alveoli fill with air during inhalation. Oxygen within the air passes through the walls of the alveoli into the blood stream. In reverse fashion during exhalation, carbon dioxide passes from the blood into the alveoli.
What does the end of the finger do on a chest x-ray?
It shines a specific wavelength of light though the end of the finger to painlessly measure the amount of oxygen. Chest x-ray: The patterns of lung damage associated with various types of interstitial lung disease are often identifiable on chest x-rays.
Is cigarette smoke a granuloma?
smoke. Interstitial lung disease related to the inhalation of cigarette smoke can occur as a spectrum of injury that includes respiratory bronchiolitis-interstitial lung disease and desquamative interstitial pneumonia. In some cases, interstitial lung disease may be associated with a collection of inflammatory cells (granuloma), ...
How to treat cardiomegaly?
It is vital that this symptom and the underlying cause of it are treated to prevent more serious damage to the heart. Treatments include medication, surgery, and lifestyle changes.
What are the conditions associated with cardiomegaly?
Managing conditions associated with cardiomegaly, such as diabetes, high blood pressure, and obstructive sleep apnea. Leading a heathy lifestyle by quitting smoking, maintaining a healthy weight, eating a balanced diet, and staying physically active.
What is cardiomegaly heart?
What to know about cardiomegaly. Cardiomegaly is an enlarged heart. It is not a disease, but a sign of another condition. Less severe forms of cardiomegaly are referred to as mild cardiomegaly. As mild cardiomegaly does not always cause symptoms, many people with a slightly enlarged heart are unaware of the problem.
What are the two types of cardiomyopathy?
There are 2 types of cardiomyopathy. Dilative cardiomyopathy: This type is characterized by a wide, poorly functioning left ventricle, which is the heart’s primary pumping chamber. Dilative cardiomyopathy is the main reason for an enlarged heart.
What is it called when the heart is enlarged?
If the heart is enlarged then this is known as cardiomegaly, which may present as mild or severe. Cardiomegaly can be caused by many conditions, including hypertension, coronary artery disease, infections, inherited disorders, and cardiomyopathies. Cardiomyopathy is a disease of the myocardium or heart muscle that causes cardiomegaly.
What is the condition where the heart becomes larger?
Pregnancy: The heart can sometimes become larger around the time of delivery. This type of cardiomegaly may be called peripartum cardiomyopathy.
Why does my heart murmur?
Heart murmur: Some of the heart’s valves may not shut correctly due to cardiomegaly. This causes a backflow of blood, which leads to sounds called heart murmurs. Heart murmurs may be harmless but should be monitored. Complications of cardiomegaly depend on the reason for it and the level of the enlargement.
How to treat mild cardiomegaly?
Keep your sodium intake under 1,500 milligrams per day. Reduce your alcohol intake. Quit smoking.
What are the risk factors for mild cardiomegaly?
Risk factors include: a family history of heart disease. a sedentary lifestyle. hypertension. diabetes. obesity. history of alcohol or drug abuse.
What does it mean when your heart is enlarged?
Cardiomegaly means an enlarged heart. Mild cardiomegaly refers to less severe forms. This is a sign of another heart-related condition. You may not know you have an enlarged heart unless you undergo imaging tests or have symptoms of the underlying condition.
What is the first line of treatment for heart problems?
Heart conditions. For heart conditions, the preferred first line of treatment is medication . Your doctor may recommend different medications for the following: atrial fibrillation: antiarrhythmic drugs and blood thinners.
How to diagnose a heart enlarged?
Diagnosing mild cardiomegaly. Imaging tests are the best way to detect an enlarged heart. These measure your heart’s size, movement of blood throughout the chambers and valves, and your heart’s electrical activity. Your doctor may order one or more of the following: echocardiogram. chest X-ray.
Is cardiomegaly serious?
Mild cardiomegaly isn’t considered as serious as moderate or severe cardiomegaly. But for all forms of cardiomegaly, the focus should be on the underlying condition. Some mild forms are temporary, such as those caused by drug and alcohol abuse. Other forms are permanent, and can progressively get worse if the underlying condition isn’t treated.
Can being overweight cause cardiomegaly?
Making sure you’re up to date on your medications for diabetes and thyroid disease can help reduce complications like cardiomegaly. If you’re overweight, losing excess pounds can make a difference, too.
What are the abnormalities in pulmonary function testing?
Pulmonary function testing. Laryngoscopy or bronchoscopy. Abnormalities include hypoxia (from bronchospasm or pulmonary edema) [ 1] and metabolic acidosis, which may be a hyperchloremic (nonanion gap) acidosis. [ 7] . It is postulated that this may be caused by the absorption of hydrochloric acid following the reaction of chlorine gas ...
Is chest radiography normal?
Chest Radiography. The chest radiograph findings are frequently normal initially but may exclude other causes of hypoxia in the differential. Abnormalities may nonspecific; however, pulmonary edema, pneumonitis, [ 33] and adult respiratory distress syndrome (ARDS) may be seen in some cases.
Clinical Presentation
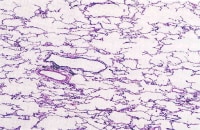
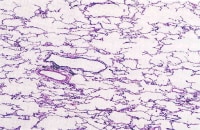
Pathology
- One method of classifying pulmonary edema is as four main categories on the basis of pathophysiology which include: 1. increased hydrostatic pressure edema 1.1. two pathophysiological and radiological phases are recognized in the development of pressure edema 1.1.1. interstitial edema 1.1.2. alveolar flooding or alveolar edema 1.2. these phases are virtuall…
Radiographic Features
- The chest radiograph remains the most practical and useful method of radiologically assessing and quantifying pulmonary edema 3,4. Features useful for broadly assessing pulmonary edema on a plain chest radiograph include: 1. upper lobe pulmonary venous diversion (stag's antler sign) 2. increased cardiothoracic ratio/cardiac silhouette size: useful ...
Differential Diagnosis
- General imaging differential considerations include other causes of diffuse airspace opacification: 1. diffuse pulmonary hemorrhage: has no dependent gradient and usually no pleural effusion 2. diffuse pneumonia 6: usually no dependent gradient 3. pulmonary alveolar proteinosis: usually no pleural effusion
See Also